Session Information
Date: Sunday, October 26, 2025
Title: Abstracts: Orthopedics, Low Back Pain, & Rehabilitation (0783–0788)
Session Type: Abstract Session
Session Time: 1:15PM-1:30PM
Background/Purpose: Physical activity (PA) and exercise therapy are guideline-supported interventions for chronic LBP, but their influence on the transition from acute to chronic LBP is unclear. This study aimed to determine if baseline self-reported exercise therapy or sufficient PA during the acute LBP phase would prevent a transition to chronic LBP at 3 or 6 months.
Methods: Participants were recruited from Durham and Kannapolis, NC communities from February to November 2022 and followed at 3 and 6 months. Participants were nonpregnant adults aged 18+ with acute LBP (< 4 weeks before screening and ≥30 days without LBP before acute onset) without systemic inflammatory or autoimmune conditions, non-skin cancer, lumbar spine surgery, low back trauma, congenital/acquired spinal defects. Baseline PA was measured via the Exercise Vital Signs (EVS) tool and dichotomized into sufficiently active (>150 minutes of moderate to vigorous PA) versus not. Baseline interventions were captured as yes/no from the NIH LBP Task Force Measure. Comorbidities were measured with the Charlson Comorbidity Index. Chronic LBP was defined as pain most/every day over the past 3 months, and high impact chronic LBP as pain limiting daily work or activities most/every day. Descriptive statistics (counts, proportions, means + SD), t-tests, or Fisher’s exact tests were used for comparisons across groups. Multiple binary logistic regression models were used to estimate odds ratios (OR) and 95% confidence intervals (CI) adjusted for age, sex, ethnicity, race, and comorbidities.
Results: We enrolled 131 participants with a transition from acute to chronic LBP of 32.2% (38/118) at 3 months and 27.9% (31/111) at 6 months. Most were female sex at birth (58.8%) with a mean age of 56.9 (SD= 13.8; range 19 to 81 years). 22.9% identified as Black/African American and 67.9% as White; 6.1% reported Hispanic ethnicity. At baseline, 39% (n=51) reported exercise therapy and 33% (n=42) were sufficiently active. These groups differed significantly (p=0.03).
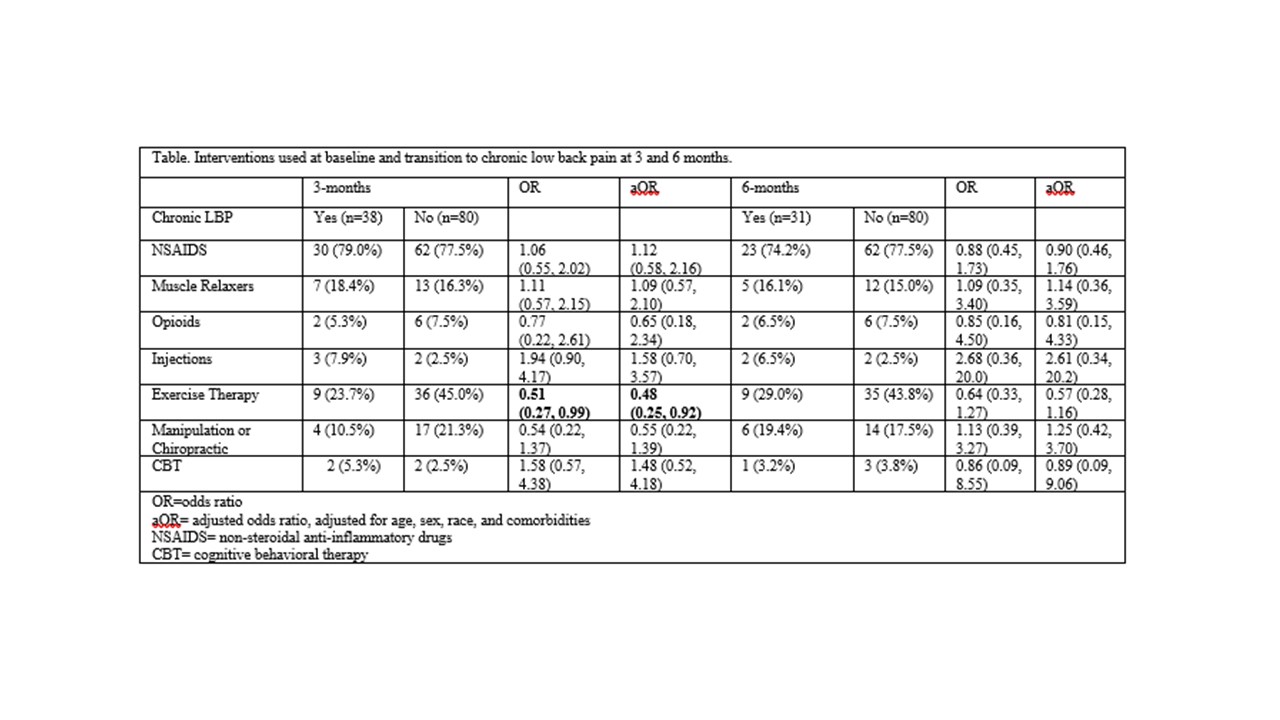
Mean baseline EVS was 125.1 minutes (limits 9, 750; median 90.0). Those who transitioned to chronic LBP had a lower mean EVS (96.9 min; range 0, 350; median 85) than those who did not (139.6 min; range 0, 750; median 100), p=0.09. Participants insufficiently active at baseline (n=6, 75% vs n=0, 0.0%, exact p< 0.001) and with lower mean exercise time (37.5 + 29.9 SD vs 122.9 + 21.6 SD; p=0.04) were more likely to transition to high impact chronic LBP at 6 months; no differences were found at 3 months. Participants using exercise therapy were 49% less likely to transition to chronic LBP (OR=0.51, 95% CI 0.27, 0.99), and the effect strengthened when adjusted for age, sex, race, and comorbidities (0.48, 95% CI 0.25, 0.92). No other intervention showed a significant association (see table).
Conclusion: This longitudinal study is the first to examine PA and exercise therapy in the transition from acute to chronic LBP in the community. Findings suggest strong clinical utility for exercise therapy in risk reduction of chronic LBP at 3 months, and PA may help prevent high impact chronic LBP at 6 months.
To cite this abstract in AMA style:
Harker K, Fillipo R, Goode A. Physical Activity and Exercise Therapy Reduce the Transition from Acute to Chronic Low Back Pain in the Community [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/physical-activity-and-exercise-therapy-reduce-the-transition-from-acute-to-chronic-low-back-pain-in-the-community/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/physical-activity-and-exercise-therapy-reduce-the-transition-from-acute-to-chronic-low-back-pain-in-the-community/