Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Prior work suggests that women with rheumatic diseases are rarely prescribed contraception. However, in addition to preventing undesired pregnancy, contraception may help these women to delay pregnancy until their diseases are well-controlled on pregnancy-compatible anti-rheumatic drugs— thus, optimizing their chances for healthy maternal and fetal outcomes. While hormonal contraception may augment thrombotic risks in diseases such as systemic lupus erythematosus and antiphospholipid antibody syndrome, most women with rheumatic diseases are able to use contraception safely. This qualitative study explored women’s perspectives about contraception use in the context of their diseases, and their preferences for contraception care from their health care providers.
Methods: Semi-structured interviews were conducted among women ages 18-45 diagnosed with at least one rheumatic disease, who were recruited from two outpatient rheumatology clinics in Pittsburgh, PA. Interviews were transcribed verbatim, and a code book was inductively developed based on transcript content. Two independent coders applied the code book to all transcripts, and coding differences were adjudicated to full agreement. The finalized coding was used to conduct a thematic analysis.
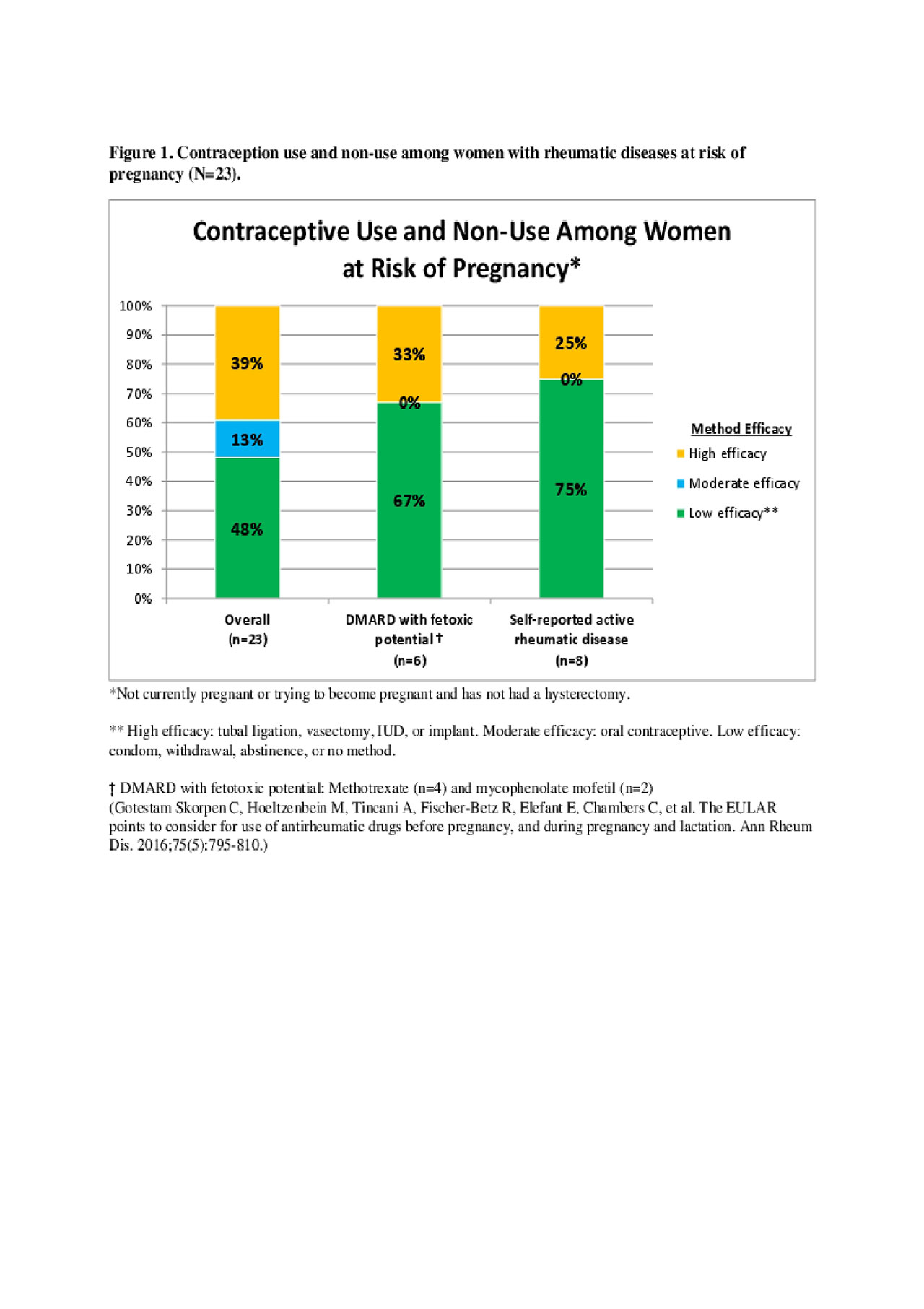
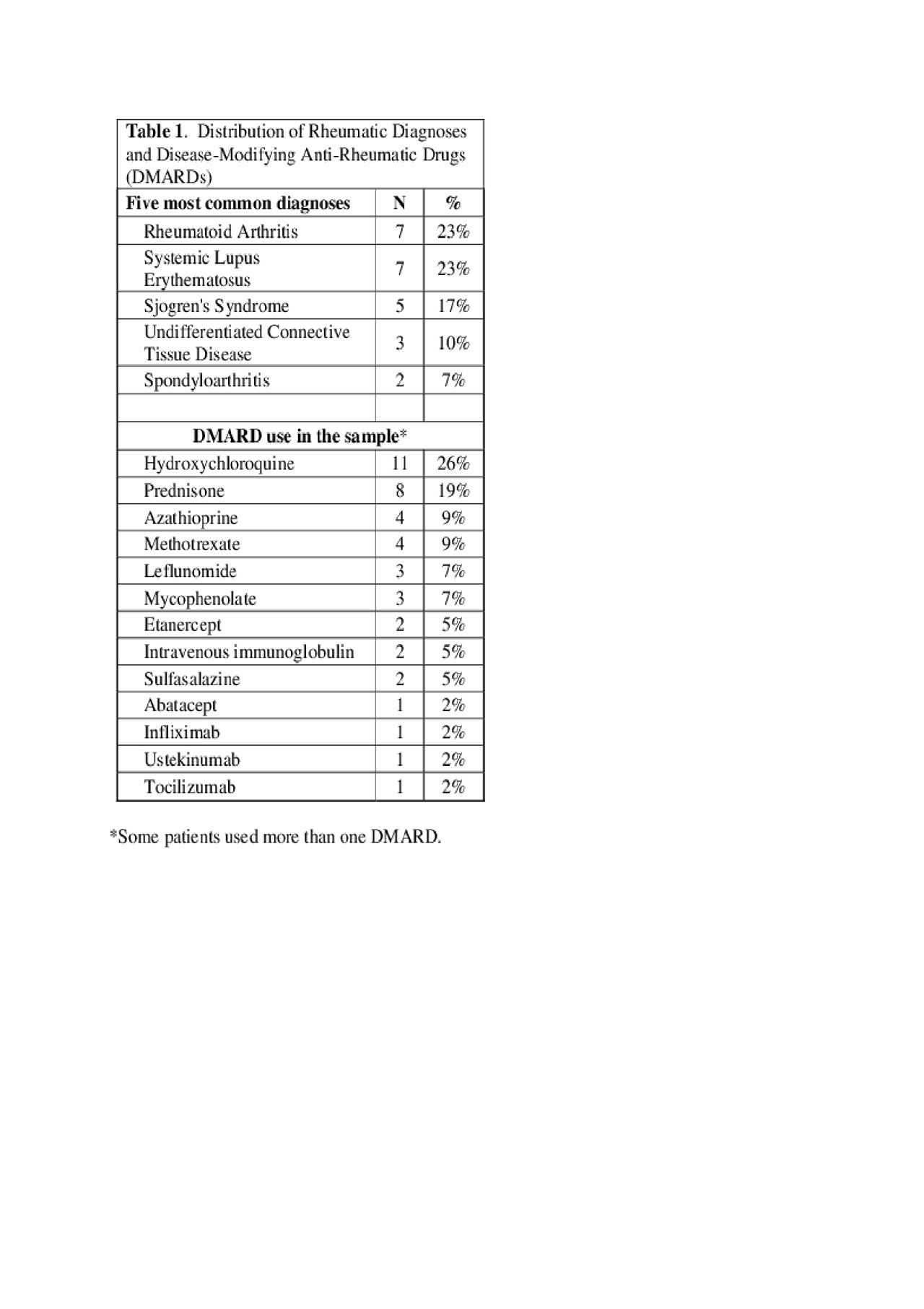
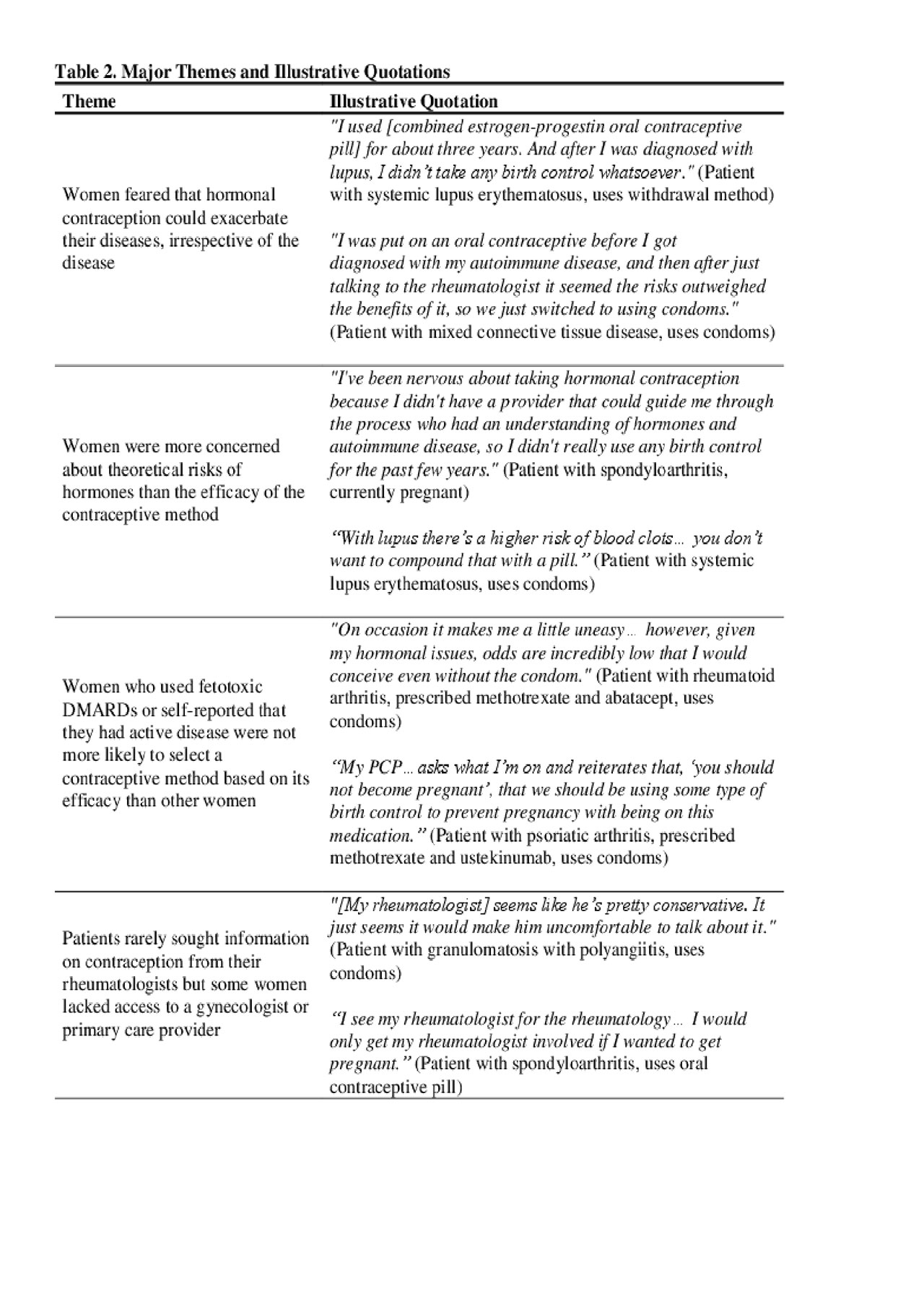
Results: Thirty women participated in interviews; the average age of the sample was 35.1 years (S.D. 5.8), and most women were white (73%), married (52%), and had at least one child (53%). Twenty-three women were at risk for pregnancy; others had a hysterectomy, were pregnant (n=2), or attempting to conceive (n=1). Table 1 presents the disease diagnoses and DMARDs used by women in the sample. Four major themes about contraception emerged from the interviews (Table 2): 1) Women feared that hormonal contraception could exacerbate their rheumatic diseases, irrespective of the disease; 2) Women were more concerned about theoretical risks of hormones than the efficacy of the contraceptive method; 3) Women who used fetotoxic DMARDs or reported that they had active rheumatic disease were not more likely to select a contraceptive method by its efficacy than other women; and 4) Patients rarely sought information about contraception from their rheumatologists but some women lacked access to a gynecologist or primary care provider. Figure 1 presents contraception methods used by women at risk of pregnancy and by women who used potentially fetotoxic DMARDs or who had active disease— i.e., elevated risk of adverse pregnancy outcomes.
Conclusion: Many women prioritized limiting their exposure to hormones rather than preventing pregnancy with hormonal contraception, including women who did not wish to become pregnant or had elevated risk of adverse pregnancy-related outcomes. Most women did not perceive that their rheumatologists were the appropriate providers to manage their contraception care, but some women lacked access to contraception providers. Our study suggests that women with rheumatic diseases may require counseling about the effects of exogenous hormones on their diseases, education about safe and efficacious contraception methods, and consistent access to contraception care.
To cite this abstract in AMA style:
Stransky O, Wolgemuth T, Chodoff A, Birru Talabi M. Perspectives About Contraception Among Reproductive-Aged Women with Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/perspectives-about-contraception-among-reproductive-aged-women-with-rheumatic-diseases/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/perspectives-about-contraception-among-reproductive-aged-women-with-rheumatic-diseases/