Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Cognitive impairment (CI) is a common manifestation of systemic lupus erythematosus (SLE) and its course may change over time. The objective was to determine the prevalence of persistent CI in SLE patients over 1 year time and investigate the associated factors.
Methods: Consecutive SLE patients, aged 18-65 years, who attended a single centre (2016- 2019) were included. Patients were administered the Neuropsychological Battery (NB) at baseline (T0), 6 months (T1) and 12 months (T2). Patients’ scores were compared to normative data to obtain z-scores. CI was operationalized on the NB as a z-score of ≤-1.5 on ≥2 domains. Three groups were identified: Persistent CI group – CI present in all 3 assessments; stable non-CI group – CI not present in all 3 assessments; or fluctuating CI group – CI was on 1-2 assessments. At each visit, data on sociodemographic, clinical and laboratory/medications were collected. Fatigue was measured by the Fatigue Severity Score (FSS), pain by the transformed scale of the Bodily Pain domain of SF-36 and anxiety by BECK Anxiety Inventory (BAI). Patients with persistent CI were compared to stable non-CI patients. Multivariable polynomial logistic regression was performed on all 3 groups to study the likelihood of a patient classified to adjunct worse group.
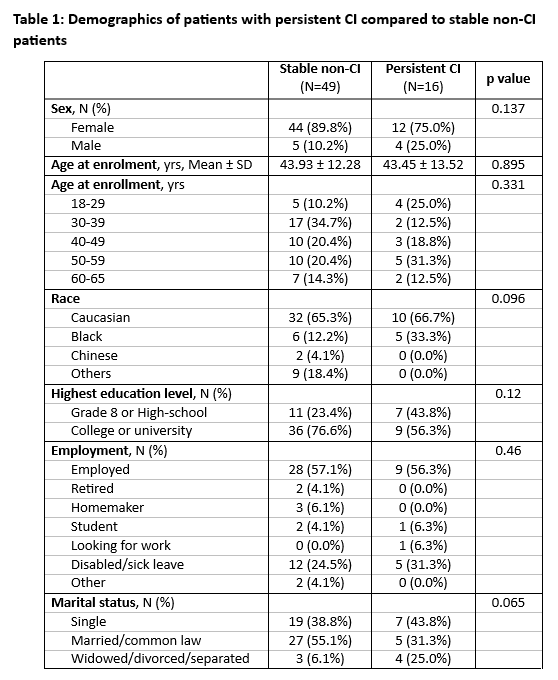
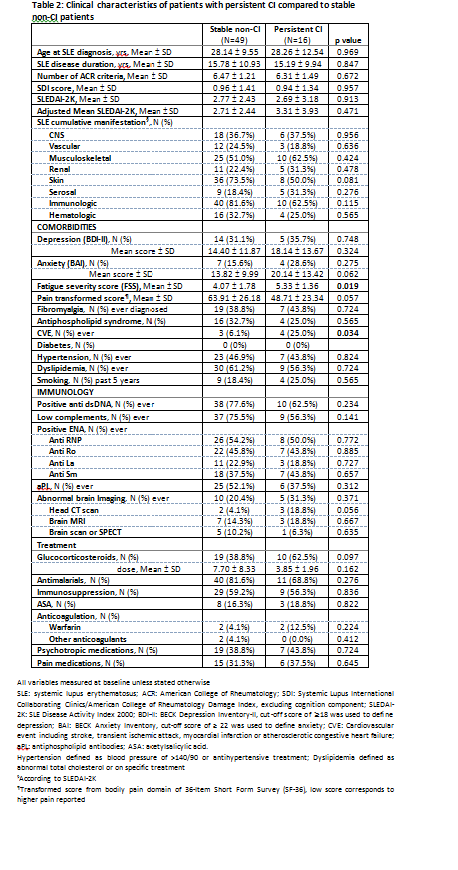
Results: The prevalence of CI was 40%, 26% and 38% at T0, T1 and T2 respectively among 111 patients who completed all 3 assessments. Sixteen patients (14%) experienced persistent CI, 46 (41%) fluctuating CI and 49 (44%) stable non-CI. Patients with persistent CI had higher proportion of male, Black, and widowed/divorced/separated patients compared to stable non-CI group (Table 1). A higher level of fatigue, pain and anxiety were identified in persistent CI group (Table 2). The persistent CI group showed higher proportions of cardiovascular events (CVEs) and abnormal brain imaging. Glucocorticoid use was higher while antimalarial use was lower in the persistent CI group with no difference in immunosuppressives, aspirin, pain or psychotropic medications. There were no differences in SLE manifestations, other comorbidities (e.g. fibromyalgia and antiphospholipid syndrome), SDI, SLEDAI-2K and immunological profile.
The Multivariate analysis on all 3 groups showed that Black [odds ratio (OR) of 2.9 (95% confidence interval: 1.1-7.7, p 0.03)] and Fatigue [OR 1.3 (1.04-1.7; p 0.02)] were associated with a higher likelihood of being classified in the adjunct worse group.
Conclusion: Persistent CI was found in 14% of the patients in all 3 assessments over 1 year. Higher proportion of male, Black, CVE, fatigue and anxiety were observed among patients with persistent CI. Black patients and fatigue were also associated with a higher likelihood of being classified in the adjunct worse group. Our results advocate for further research into the associated factors with CI persistence in SLE patients. This demonstrates the complexity of the underlying factors associated with persistence CI – genetic/epigenetic, disease severity, sociodemographic, comorbidities (fatigue, anxiety, etc.), which requires further research.
To cite this abstract in AMA style:
Beaton D, Green R, Ruttan L, Wither J, Tayer-shifman O, Tartaglia M, Kakvan M, Anderson N, Su J, Zandy M, Choi M, Fritzler M, Touma Z. Persistent Cognitive Impairment in Lupus Patients over 1 Year and Associated Factors [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/persistent-cognitive-impairment-in-lupus-patients-over-1-year-and-associated-factors/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/persistent-cognitive-impairment-in-lupus-patients-over-1-year-and-associated-factors/