Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: A thrombosis risk score containing abnormal Platelet-bound C4d (PC4d), low complement C3 and abnormal anti-phosphatidyl serine prothrombin (PS/PT) IgG antibody has been shown to associate with thrombosis in Systemic Lupus Erythematosus (SLE). Our objective was to evaluate the relationships between persistency in PC4d, risk score and thrombosis during follow-up (FU). A secondary objective evaluated the impact of whole blood Hydroxychloroquine (HCQ) levels in associating with thrombosis.
Methods: This was a longitudinal study of 149 SLE patients (mean age: 47±1 years, 86% female), with (n=16, 11%) or without (n=132, 89%) a history of thrombosis (venous or arterial) in the past 5 years. PC4d was measured using flow cytometry. Percent FU visits with abnormal PC4d status ( >20 mean fluorescence intensity [MFI]) was calculated. Persistency in PC4d was defined as abnormal PC4d ( >20 net MFI) status at baseline and all FU visits, intermittent PC4d was defined as abnormal PC4d status during at least one visit. Complement C3 (< 81 mg/dl) and anti-PS/PT IgG ( >30 Units) were measured using immunoassays. Mean thrombosis risk score for each patient was calculated. Whole blood HCQ levels were measured using liquid chromatography and mean HCQ per patient was calculated. Statistical analysis consisted of Wilcoxon, Fisher’s Exact and logistic regression. Odds Ratio (OR) with confidence intervals (CI) were calculated.
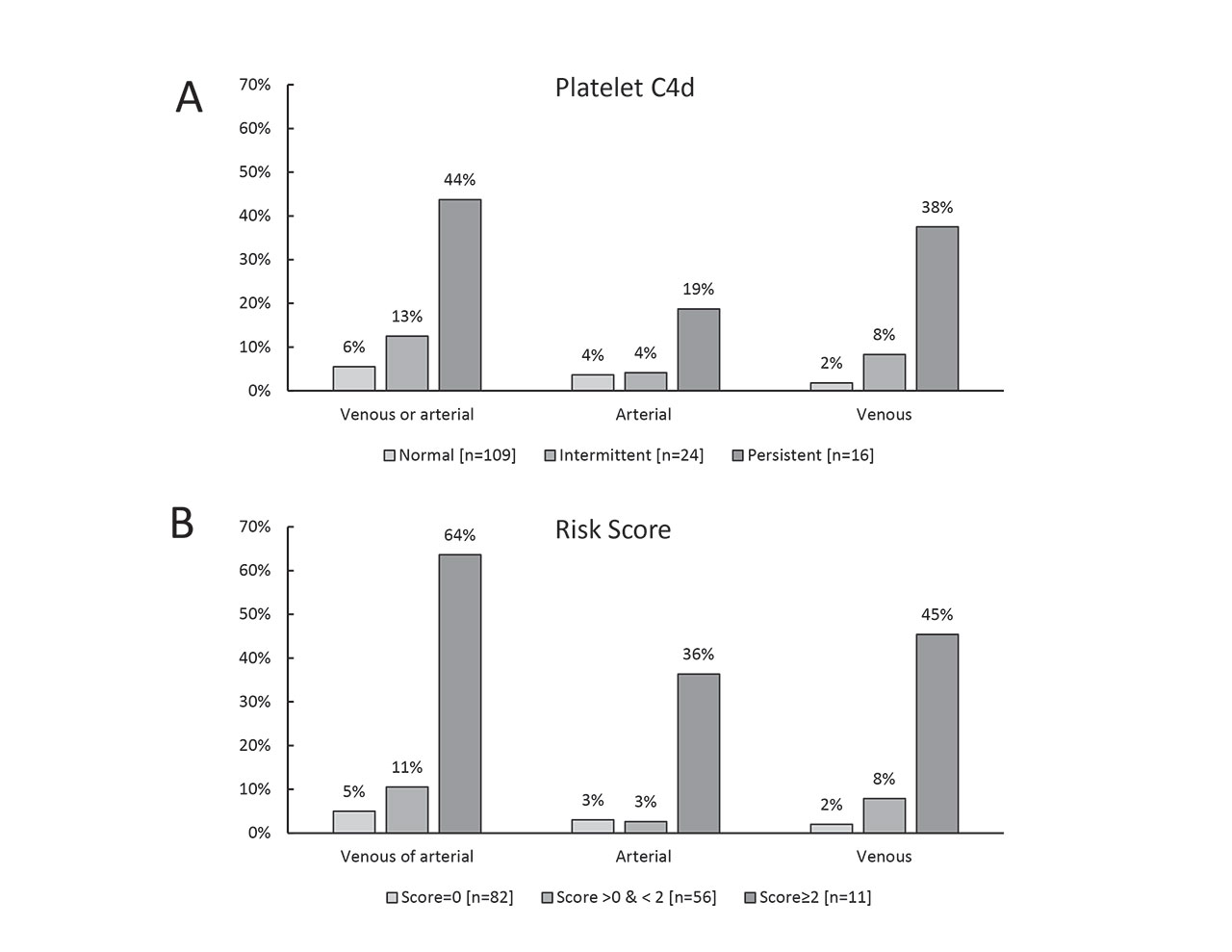
Results: 424 FU visits were collected (average 3 visits per patient). Persistent and intermittent PC4d status were observed in 16 (11%) and 24 patients (16%), respectively. Logistic regression analysis revealed that the percentage FU visits with abnormal PC4d status significantly associated with any thrombosis (OR range 11.7 CI 95%: 3.23-42.44) (p< 0.001), venous thrombosis (OR range= 33.4 CI95: 5.8-193.5) (p< 0.001) and approached significance with arterial thrombosis (OR=4.7 CI 95%: 0.9-25.4) (p=0.08) (Figure 1, panel A). During FU, the mean risk score per patient was 0.57±0.76 (n=149). Risk score at FU associated with any thrombosis (OR= 3.8 CI 95%: 2.0-7.2 per unit change, OR range = 53.9 CI 95%: 7.8-372.4) (p< 0.001), venous thrombosis (OR= 3.9 CI 95%: 1.9-8.2 per unit change, OR range = 60.3 CI95%: 6.5-560.8) and arterial thrombosis (OR= 3.0 CI95%: 1.4-6.4 per unit change, OR range = 26.5 CI95%: 2.7-259.4) (Figure 1, panel B). Among 133 patients treated with HCQ, median HCQ levels were 696 ng/ml (Interquartile range [IQR]: 537-989 ng/ml, n=15), 794 ng/ml (IQR: 628-1121 ng/ml, n=22), and 976 ng/ml (IQR: 675-1300 ng/ml, n=96) in the group of patients presenting with persistent, intermittent and normal PC4d status, respectively. Levels were significantly lower in the group of patients with persistent or intermittent PC4d status when compared to normal PC4d (p=0.028). Risk score did not associate with HCQ levels. Lower HCQ levels tended to associate with venous thrombosis (median=916 ng/ml [IQR: 675-1300], n=10 vs 648 ng/ml [IQR: 382-929], n=123) (p=0.061) but not with arterial thrombosis (p >0.20).
Conclusion: Our data suggest that persistency in PC4d and the thrombosis risk score both associate with thrombosis. Lower HCQ levels may associate with venous thrombosis.
To cite this abstract in AMA style:
Petri M, Conklin J, O'Malley T, Ligayon J, Wolover L, Dervieux T. Persistency in Platelet C4d and Thrombosis Risk Score Associate with Thrombosis in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/persistency-in-platelet-c4d-and-thrombosis-risk-score-associate-with-thrombosis-in-systemic-lupus-erythematosus/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/persistency-in-platelet-c4d-and-thrombosis-risk-score-associate-with-thrombosis-in-systemic-lupus-erythematosus/