Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
Among many other organs and systems, ANCA-associated vasculitis (AAV) may also affect nervous system in up to more than half of patients, resulting in various central nervous system (CNS) disturbances and/or involvement of cranial or peripheral nerves. In the present study, we focused on pure peripheral neuropathy and aimed to compare the frequency of this problem between patients having microscopic polyangiitis (MPA) with those having granulomatosis with polyangiitis (GPA).
Methods:
Medical charts of 48 patients with MPA and 58 patients with GPA, fulfilling relevant European Medicines Agency (EMA) classification algorithm, and being followed up by Ege University Hospital Rheumatology Department between 1997 and 2017 were retrospectively analyzed. Presence or absence of symptoms suggesting peripheral sensorial and/or motor neuropathy and electromyography (EMG) results were noted. Additional co-morbidities which may cause neuropathy such as diabetes mellitus were also noted. Patients with CNS problems and/or cranial nerve(s) involvement were excluded. Descriptive analyses were given using mean ± standard deviation (SD) for continuous variables and numbers (percentages) for categorical variables. Chi-square test was used to analyze differences between categorical data, while Mann-Whitney U tests were applied to test statistical differences between continuous data.
Results:
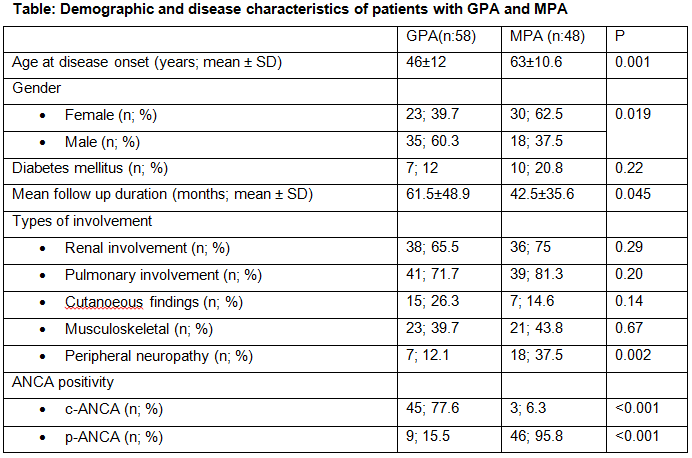
Demographic features, mean follow up durations, types of clinical involvements, and ANCA status of the patients are given in Table. Patients with MPA were notable with being more frequently women and having older age of disease onset. Frequency of peripheral neuropathy in MPA (37.5%) was significantly higher than in GPA (12.1%). Peripheral neuropathy was in the form of axonal sensorimotor type in all patients, except for two cases with MPA having pure motor neuropathy. The frequency of diabetes in both groups was not statistically different. On the other hand, comparison of all patients with and without peripheral neuropathy showed that peripheral neuropathy group had older age of disease onset (60.88±13.6 versus 51.7±13.73 years, p:0.04) and had more frequent musculoskeletal symptoms (39.7% versus 33.3%, p:0.02).
Conclusion:
Our data show that peripheral neuropathy is more frequent in patients with MPA compared to GPA. In literature, there are controversial reports about whether neuropathy is more frequent in GPA or in MPA. This may be due to genetic differences, as well as inclusion or exclusion of cases with central nervous system involvement and/or cranial neuropathy. Future studies with larger series will probably clarify this issue.
To cite this abstract in AMA style:
Taş MN, Kara M, Ketenci S, Pekdiker M, Durusoy R, Bademkıran F, Keser G, Aksu K. Peripheral Neuropathy Is More Common in Microscopic Polyangiitis Than in Granulomatosis with Polyangiitis: Data from a Single Tertiary Referral Center [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/peripheral-neuropathy-is-more-common-in-microscopic-polyangiitis-than-in-granulomatosis-with-polyangiitis-data-from-a-single-tertiary-referral-center/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/peripheral-neuropathy-is-more-common-in-microscopic-polyangiitis-than-in-granulomatosis-with-polyangiitis-data-from-a-single-tertiary-referral-center/