Session Information
Date: Tuesday, November 12, 2019
Title: Orthopedics, Low Back Pain, & Rehabilitation Poster – ACR/ARP
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Over 7 million Americans are estimated to suffer from inflammatory rheumatologic diseases and the rate of joint arthroplasties are nearly 50 % higher among this population as compared to controls. Many of these patients are on glucocorticoids around the time of their joint surgeries. The optimum perioperative management of glucocorticoid dosing is not known and there is no established clinical practice. The most recent recommendation by American College of Rheumatology/ American Association of Hip and Knee Surgeons to continue home steroid dose rather than administer supraphysiologic stress dose for patients undergoing elective arthroplasties was based on a low level of evidence. The aim of our study was to compare the rates of peri- and postoperative outcomes after elective joint arthroplasties with continuing home glucocorticoid dosing versus administering stress dose steroid.
Methods: The study is a retrospective case-control study done at the Reading Hospital. Hospital records were used to select patients who were had elective joint arthroplasties (in 5 years period from February 2013- July 2018) and concomitant rheumatologic diseases on chronic steroids. The patients with rheumatologic diseases that received stress dose steroid in the perioperative period (cases) and did not receive stress dose steroid (control) were identified. Patient-specific demographic and clinical data and information on perioperative and postoperative outcomes were extracted.
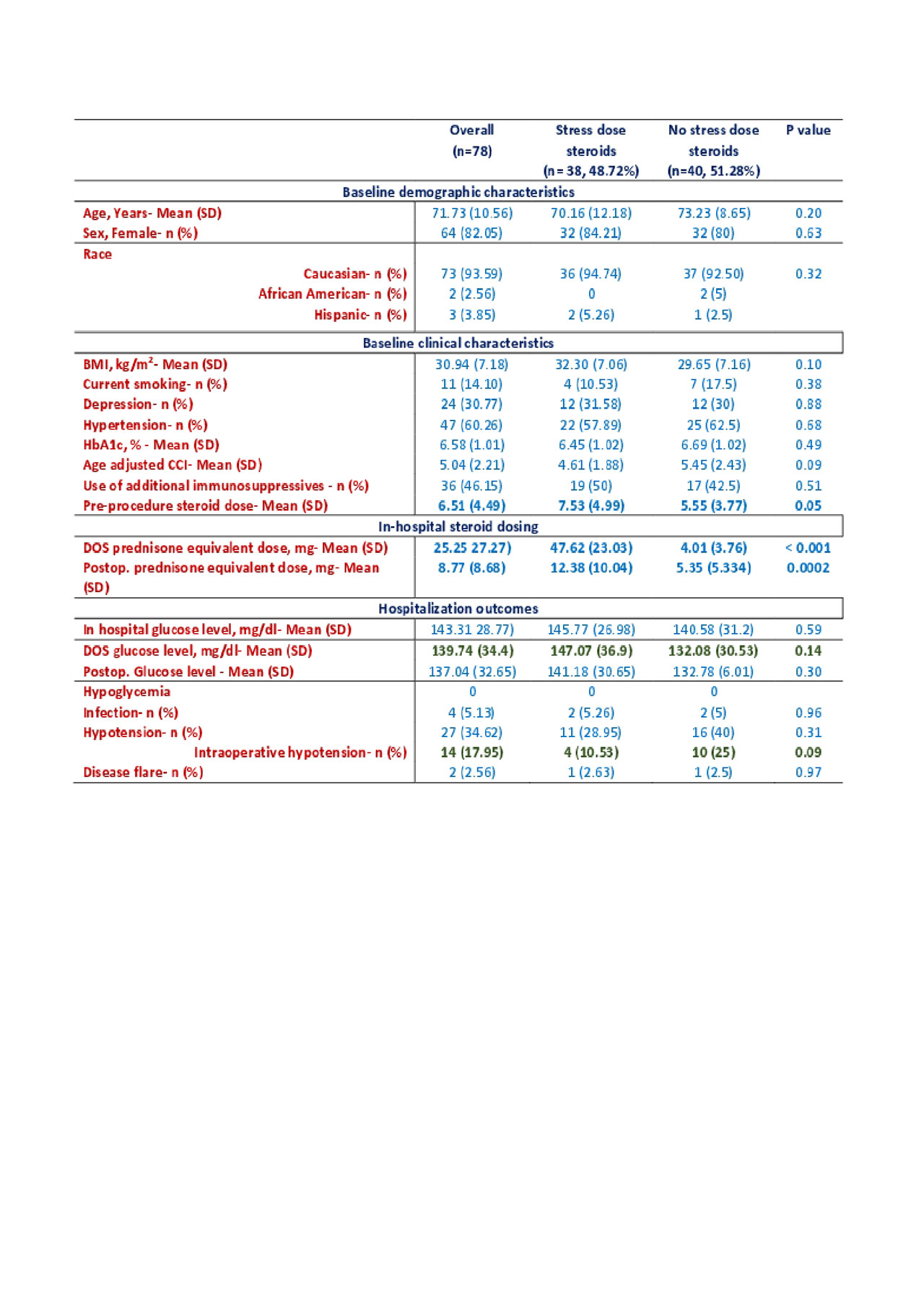
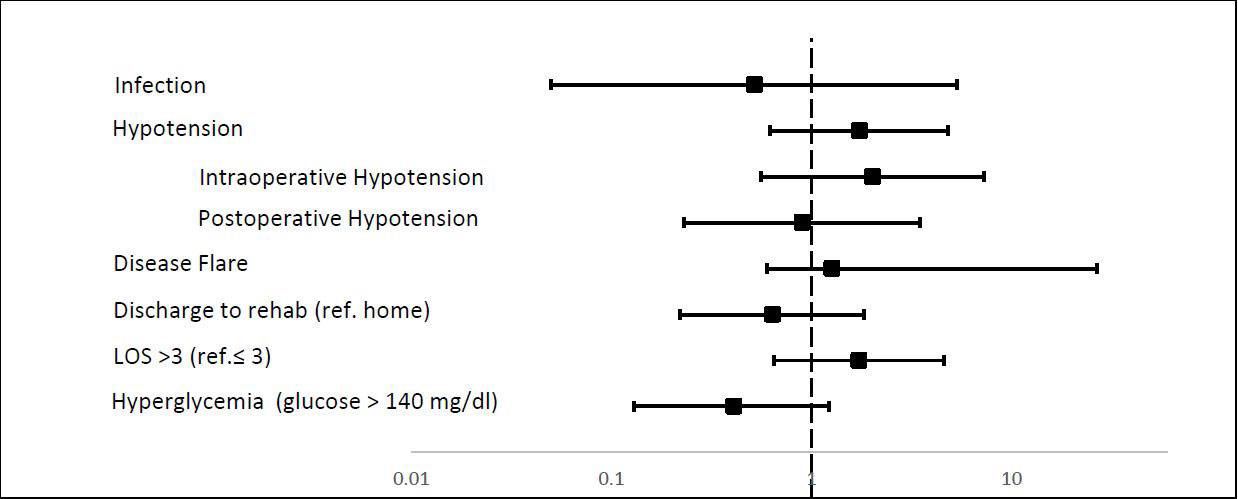
Results: 78 patients met the inclusion criteria, among which about 49 % received stress dose steroids perioperatively. Baseline characteristics were similar between the cases and controls (Table 1). The rate of peri- and postoperative outcomes were not significantly different between the two groups (Figure 1). Intraoperative hypotension was slightly higher in the control group versus those who received stress dose steroid (25 % vs 10.5%, p=0.09). Slight hyperglycemia was noted in the stress dose steroid group (mean in-hospital glucose 142 mg/dl vs 129mg/dl, p=0.07). No perioperative hypoglycemia was noted in either group (Table 1).
Conclusion: Although there is no clear guideline on perioperative glucocorticoid management for patients on chronic steroids, the recommended approach has been to treat patients with a high risk of secondary adrenal dysfunction (patients on > 20 mg prednisone equivalent daily for 3 weeks or with features of Cushing’s syndrome). In our study of elective joint surgeries, no stress dose steroid group had a slightly increased tendency toward intraoperative hypotension and stress dose steroid group had increased hyperglycemia. No significant hemodynamic difference was noted between the two groups. Our study had a small size and is underpowered to make conclusions, however, the paucity of evidence necessitates more adequately powered studies to compare perioperative steroid strategies.
Comparison of baseline characteristics, steroid dosing, and perioperative outcomes after elective joint surgeries in patients with rheumatologic diseases
* Odds adjusted for age, home steroid dose, use of other immunosuppressive and age-adjusted Charlson comorbidity index-
To cite this abstract in AMA style:
Dhital R, Sharma P, Mir I, Donato A. Perioperative Glucocorticoid Management in Patients with Rheumatologic Diseases Undergoing Elective Joint Surgeries [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/perioperative-glucocorticoid-management-in-patients-with-rheumatologic-diseases-undergoing-elective-joint-surgeries/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/perioperative-glucocorticoid-management-in-patients-with-rheumatologic-diseases-undergoing-elective-joint-surgeries/