Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Enthesitis is a hallmark feature of Spondyloarthritis (SpA), and frequently localizes at the Achilles tendon1. Enthesitis is predominantly measured with clinical scores like Leeds Enthesitis Index (LEI), however, magnetic resonance imaging (MRI) might represent a more sensitive tool to recognize enthesitis in both, bone and soft tissues2, providing insight about the potential disconnect between pain at entheseal sites and objective inflammation. ACHILLES is the largest double blind, placebo-controlled, multicenter Phase 3 trial to date, designed to investigate enthesitis by clinical and imaging assessments in patients (pts) with active SpA. Here, we present the MRI parameters of the heel (evaluated by central readers) in pts who were not included in ACHILLES based on a negative MRI evaluation of the (local) investigator.
Methods: Pts (≥18 years) with active SpA (peripheral or axial) had to present in ACHILLES with clinical (LEI) and MRI-positive heel enthesitis (interpreted by either the local radiologist or rheumatologist), defined as enthesitis with/without bursitis and/or bone marrow edema with/without concomitant erosions in the area of the Achilles’ tendon insertion and/or the plantar aponeurosis. The present analysis included heel MRI characteristics of pts who failed to meet the MRI study inclusion criteria based on local MRI evaluation. The MRIs of screen-failed pts were evaluated by two independent central readers, blinded to any screen failure reason, in a consensus read fashion. Centralized reading of the heel MRIs was performed according to the Psoriatic arthritis magnetic resonance imaging scoring system (PsAMRIS)3. Since PsAMRIS was developed initially for the hands, additional parameters were introduced to allow for more accurate representation of the heel: a) bone oedema (with 1-33% of bone oedematous) were further specified by oedema length ≤/ >0.5 cm and b) bone erosions were further specified by assessing the localization.
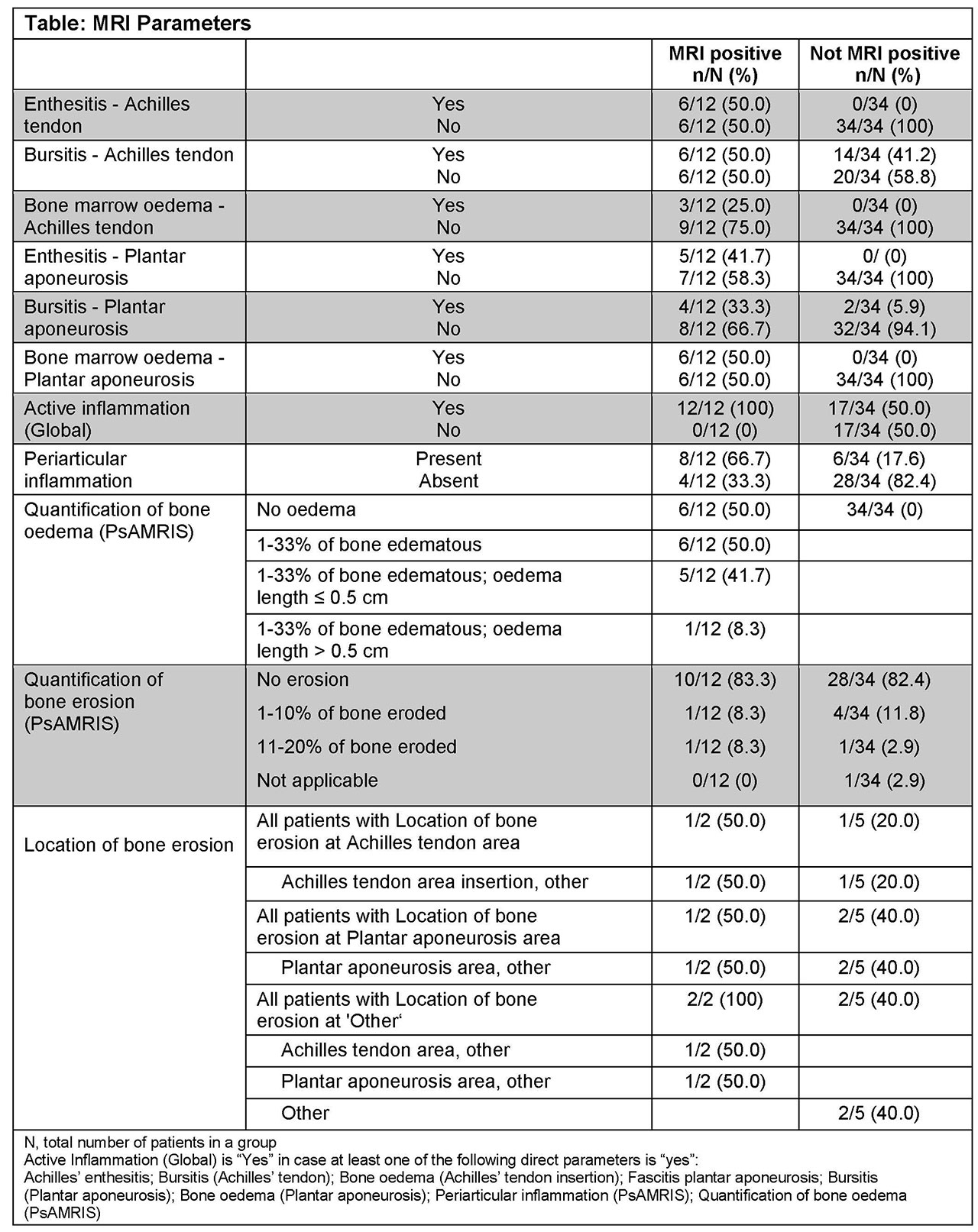
Results: Overall, 204 (128 PsA and 76 axSpA) pts were randomized and 94 pts failed screening. Of the 94 screen-failed pts, 46 pts failed due to MRI negative heel enthesitis as assessed by investigators. Upon assessment by central readers, 12/46 (26.1%) were found to be MRI positive and 34/46 (73.9%) MRI negative for heel enthesitis; MRI parameters of both groups are shown in the Table. Overall, 8/12 (67%) MRIs evaluated for positive enthesitis presented with periarticular inflammation and 6/12 (50%) with bone oedema. PsAMRIS based quantification of bone oedema revealed 1-33% of bone edematous for 6 cases, with only 1/6 having an oedema length of >0.5 cm. Enthesitis was centrally read in 6/12 (50%) MRIs at the Achilles tendon insertion and in 5/12 (42%) at the Plantar aponeurosis calcaneal insertion.
Conclusion: In central reading, concomitant periarticular inflammation and bone marrow oedema at the tendon insertion were found to be critical for the confirmation of enthesitis on MRI in patients suffering from SpA.
References:
- Schett G, et al. Nat Rev Rheumatol. 2017;13:731─41.
- PoggenborgRP, et al. Ann Rheum Dis. 2015;74:823─9
- Ostergaard M, et al. J Rheumatol. 2009;36:1816─24
To cite this abstract in AMA style:
Baraliakos X, Sewerin P, de Miguel E, Kleinmond C, Shekhawat A, Wiedon A, Behrens F. Periarticular Inflammation and Bone Marrow Oedema Are Important in the Evaluation of Enthesitis on MRI in Patients with Peripheral and Axial SpA [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/periarticular-inflammation-and-bone-marrow-oedema-are-important-in-the-evaluation-of-enthesitis-on-mri-in-patients-with-peripheral-and-axial-spa/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/periarticular-inflammation-and-bone-marrow-oedema-are-important-in-the-evaluation-of-enthesitis-on-mri-in-patients-with-peripheral-and-axial-spa/