Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Renal involvement in ANCA-associated vasculitides (AAVs) is an important factor for morbidity and mortality. Berden’s histopathologic classification for ANCA-associated glomerulonephritis has been proven to be helpful for predicting the renal outcome. Recently, the ANCA renal risk score, a new scoring system which needs to be validated, has been proposed to predict end-stage renal disease (ESRD) in AAV patients. In this study, we aimed a) to assess prognostic factors for renal survival in our AAV patients with renal involvement, b) to evaluate the performances of the Berden’s histopathological classification and ANCA-renal risk score, for predicting ESRD.
Methods: Patients with AAV who were categorized according to the 2012 Chapel Hill consensus nomenclature were included in this study. Patients with only renal involvement clinically and diagnosed by renal biopsy were classified as renal-limited vasculitis (RLV). Renal biopsies were reviewed according to the Berden’s histopathological classification, and the percentages of normal glomeruli, tubular atrophy and interstitial fibrosis were determined in order to calculate ANCA renal risk score. The clinical data and laboratory parameters were collected retrospectively. Renal survival was defined as the time between diagnosis and the development of ESRD. Factors predictive of renal survival were evaluated by Kaplan-Meier method and the Cox proportional hazard model.
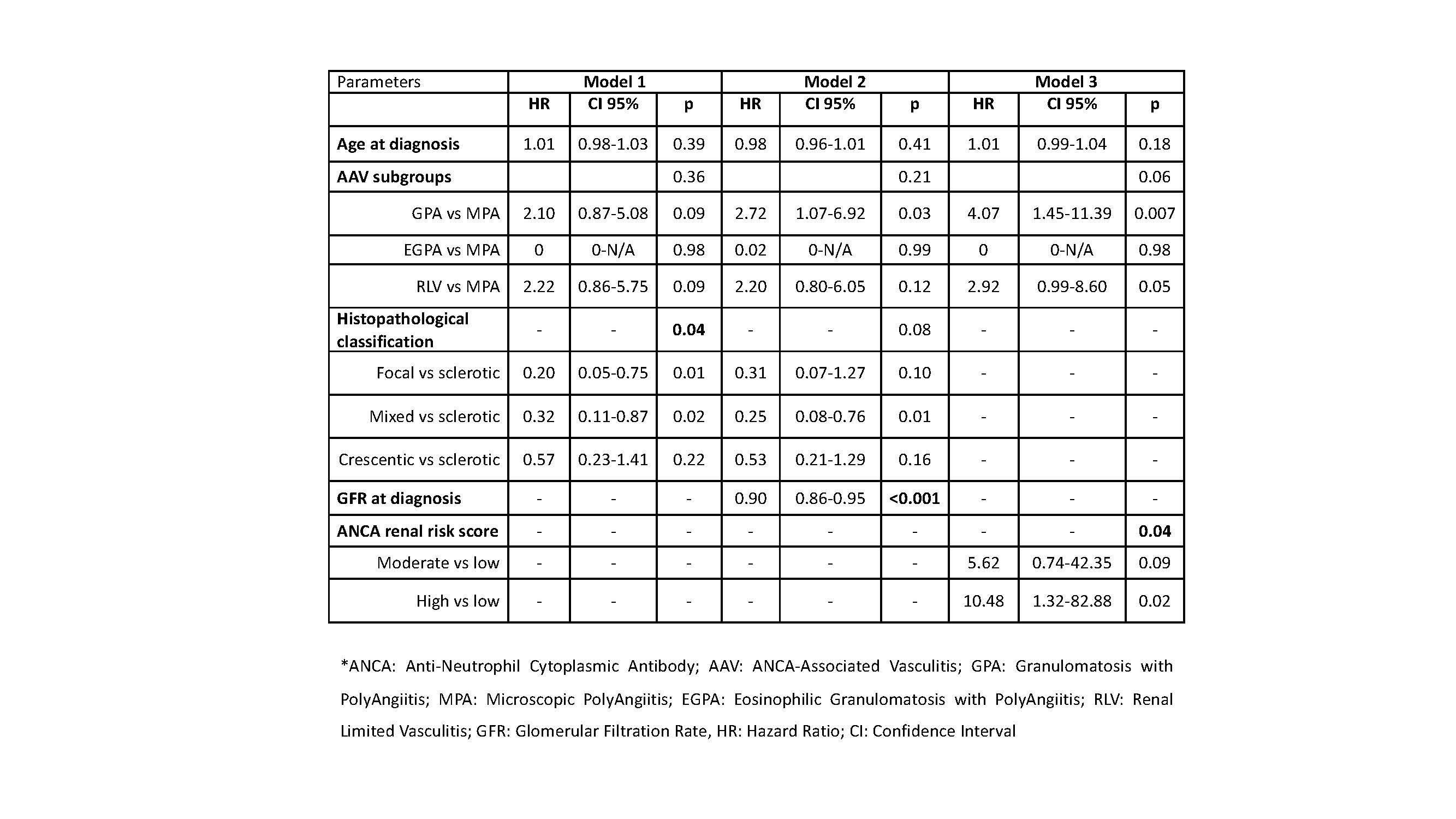
Results: 167 AAV patients with renal involvement were included in the study. ESRD had developed in 52 (34%) patients and renal survival was median 31 (0-240) months. According to the histopathological classification ESRD had developed in %79 patients in the sclerotic group, % 51 patients in the crescentic group, %32 patients in the mixed group and %18 patients in focal group (p=0.003). According to the ANCA renal risk score, ESRD had developed in %8 patients in the low-risk group, %42 patients in the medium-risk group and %67 patients in the high-risk group (p=0.005). In univariate analysis the age at diagnosis (HR 1.02, 95 % CI 1.00-1.04, p=0.045), AAV subgroups (p=0.01) (Figure), histopathological classification (p=0.009), ANCA renal risk score (p=0.01), maximum creatinine level at diagnosis (HR 1.14, 95 % CI 1.09-1.19, p< 0.001), glomerular filtration rate (GFR) (HR 0.92, 95 % CI 0.89-0.95, p< 0.001), hemodialysis (HR 4.81, 95 % CI 2.53-9.17, p< 0.001) and plasmapheresis at diagnosis (HR 2.36, 95 % CI 1.32-4.22, p=0.004) were the factors associated with renal survival. In multivariate analysis, histopathological classification predicted mortality in model 1, but when GFR at diagnosis is included in the model (model 2), the model lost its significance. However, the ANCA renal risk score was found to be an independent prognostic risk factor for renal survival (model 3, table 2).
Conclusion: According to our results, the ANCA renal risk score may be more advantageous in predicting ESRD development compared to Berden’s histopathological classification, and this may be due to the inclusion of glomerular filtration in scoring.
« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/performance-of-berdens-classification-and-anca-renal-risk-score-for-the-prediction-of-end-stage-renal-disease-in-anca-associated-vasculitis/