Session Information
Date: Sunday, November 8, 2015
Title: Health Services Research I: Digital Health and Patient, Provider Factors in Rheumatic Disease
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose:
Physicians often encounter patients who are treated with immunosuppressive
agents and must consider the risk of infection that the medications may pose. We
explored physician perceptions of the infectious risk of commonly used immunosuppressive
therapies, hypothesizing that they vary by specialty and level of experience.
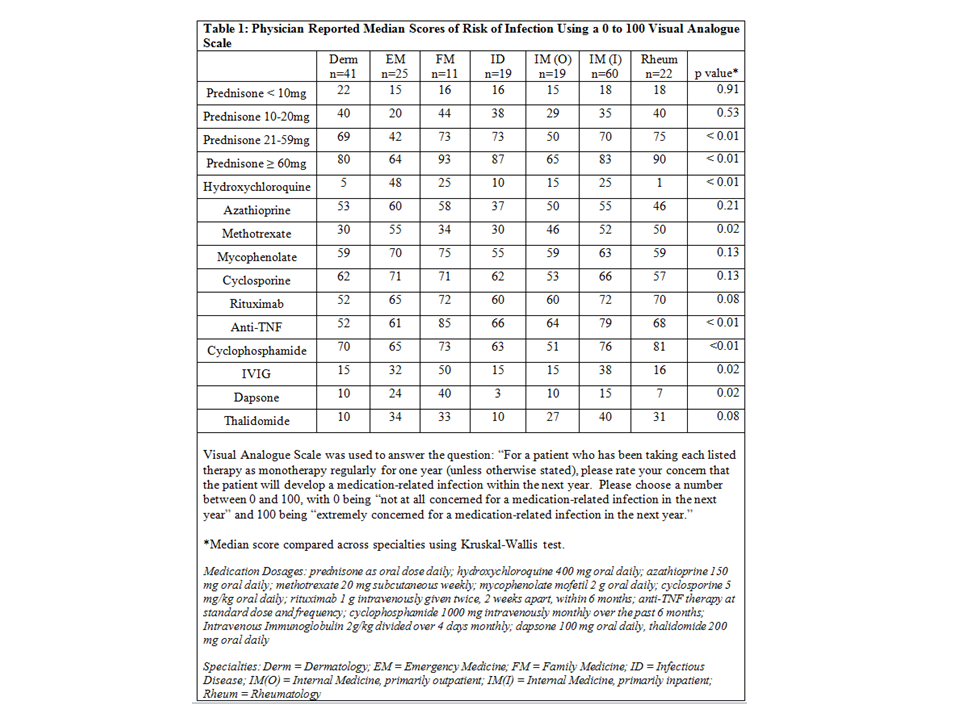
Methods: All physicians in seven departments at a
single tertiary care institution were asked to complete a web-based
survey. Data regarding medical specialty,
level of experience, years of experience post medical school, frequency of
prescribing immunosuppressant medications, and comfort level with issues
related to immunosuppressant medications were collected. Respondents were asked to rate medications
from 0 to 100 on their perception of the one-year risk of infection
attributable to that medication if used as monotherapy. To facilitate comparisons, scores were
divided into three groups, with 0 to 33 labeled low risk,
34 to 66 medium risk, and 67 to 100 high risk. Experienced physicians were defined
as those with five years of experience post medical school who also reported
that they prescribed immunosuppressant medications sometimes or
frequently.
Results:
The survey was distributed to 634 physicians; 197 physicians completed the
survey. There was a significant difference in the median rating between
specialties for 8 of 15 medications (Table 1).
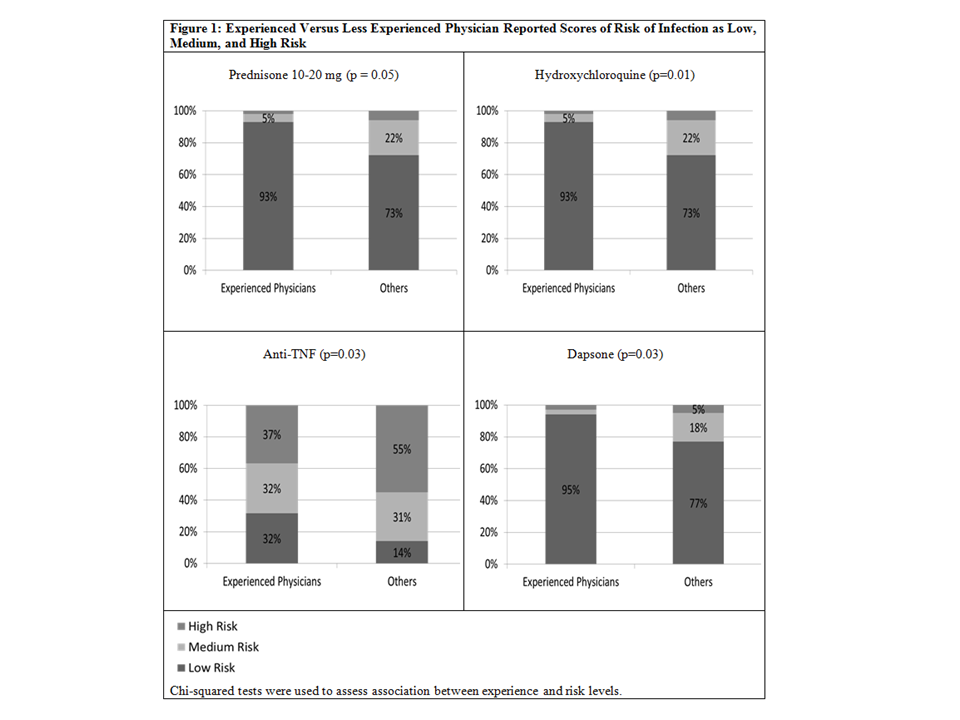
Compared to less experienced providers, the experienced providers (n=43)
generally rated hydroxychloroquine, dapsone, and anti-TNF therapy lower in
terms of infection risk (Figure 1). In contrast, 66% of experienced physicians
compared to 52% of less experienced physicians rated prednisone 10-20 mg as
medium or high risk. The majority of less
experienced physicians (55%) identified anti-TNF therapy as high risk, while
experienced physician perceptions were split nearly evenly among low (32%),
medium (32%), and high risk (37%).
Conclusion:
There is wide variability in physician perception of the infectious risk of
many immunosuppressive medications by specialty and level of experience. Among
experienced physicians who prescribe these agents, level of concern about
commonly used therapies such as anti-TNF therapy range broadly. Less experienced physicians may perceive a
lower risk of intermediate doses of prednisone and a higher risk of dapsone and
hydroxychloroquine compared to more experienced physicians. Resources to better
define and communicate the risks of immunosuppressive medications would
facilitate better care of patients who require these drugs.
To cite this abstract in AMA style:
Sharim R, Mathew L, George M, Thomas P, Rosenbach M. Perceptions of Infectious Risk of Immunosuppressive Medications Among Treating Physicians [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/perceptions-of-infectious-risk-of-immunosuppressive-medications-among-treating-physicians/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/perceptions-of-infectious-risk-of-immunosuppressive-medications-among-treating-physicians/