Session Information
Date: Monday, November 11, 2019
Title: 3S082: SLE – Clinical II: Flares & Morbidity of SLE (1824–1829)
Session Type: ACR Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: A new posited framework for categorizing patients with systemic lupus erythematosus (SLE) is the division of symptomatology into two groups: type 1 manifestations represent classic signs and symptoms of lupus, link to immune-mediated inflammatory pathways, and respond to immunosuppressive therapy; type 2 manifestations represent symptoms such as fatigue, widespread pain, cognitive dysfunction, and self-reported disease activity that do not respond to the same treatments and are an area of major unmet need1. The pathogenesis and risk factors for type 2 symptoms remain poorly defined, and prior studies suggest a possible link between stress and disease severity in SLE. We examined whether high levels of psychological stress were associated with worse disease status in SLE and whether the association differed for type 1 and type 2 symptoms.
1. Pisetsky et al. A Novel System to Categorize the Symptoms of SLE. Arthritis Care Res 2018.
Methods: Participants in this sample, drawn from the California Lupus Epidemiology Study (CLUES), were at least 18 years old and met ACR criteria for SLE. In this cross-sectional study, stress was measured using the 4-item Perceived Stress Scale (PSS, range 0-16). No cut-points have been defined for the PSS and therefore participants with scores in the top quartile were identified as those with higher stress. Type 1 symptoms were represented by the physician assessed SLE disease activity index (SLEDAI) and type 2 symptoms by self-report disease activity (SLE Activity Questionnaire, SLAQ), cognitive function (PROMIS cognitive ability scale), pain (SF-36 Bodily Pain subscale), and fatigue (SF-36 Vitality subscale). We used multivariable linear regression to evaluate the associations of stress with SLEDAI and type 2 symptoms while controlling for potential confounders (age, sex, race, education, income, smoking, disease duration, and disease damage). We then calculated adjusted means for each outcome based on the multivariable regression.
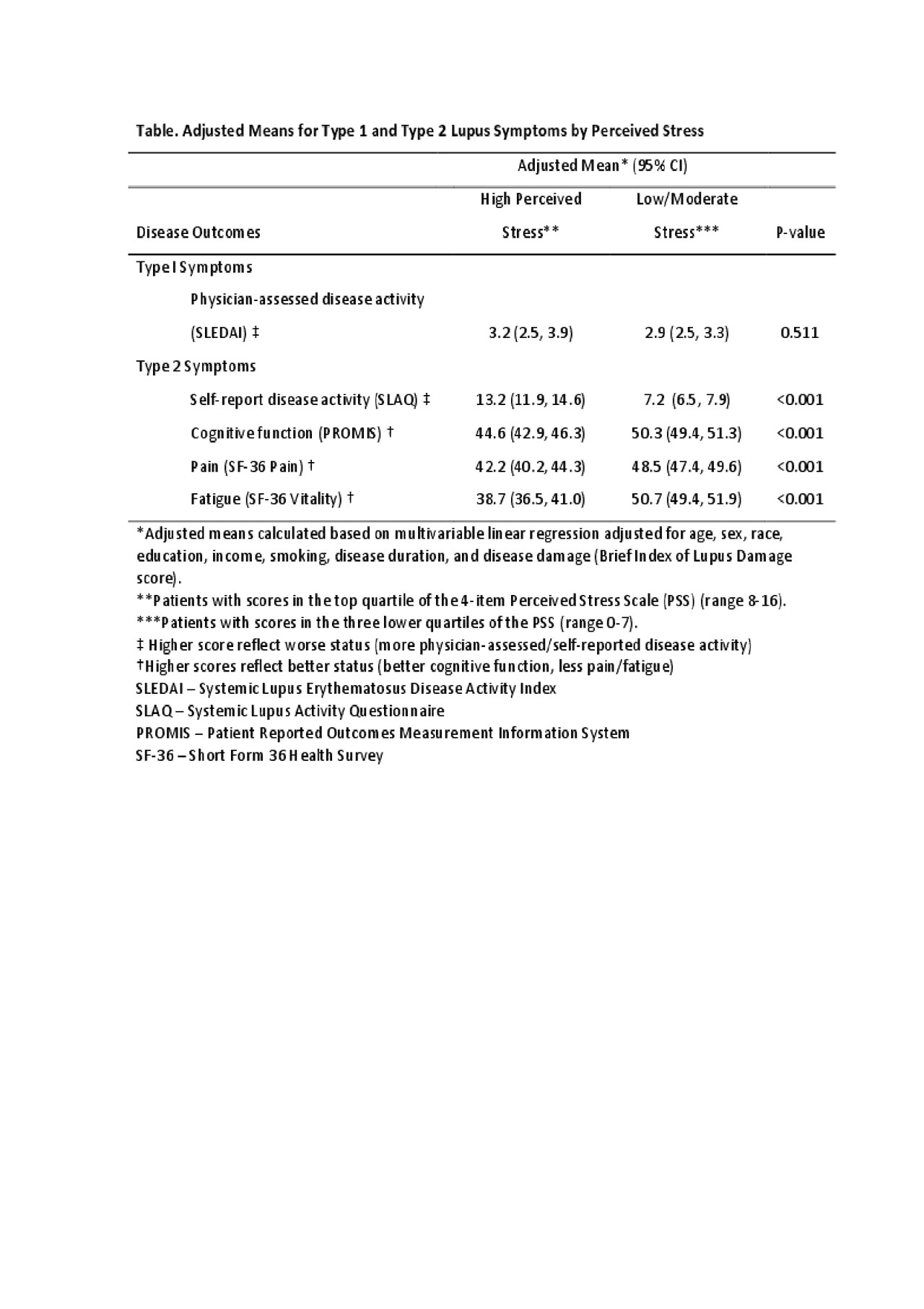
Results: The sample (n=431) was 90% female, 30% white, 34% Asian, 22% Hispanic, and 11% African American; mean age 47 (± 14) years; 19% with poverty-level income; 73% with education beyond high school; mean disease duration 18 (± 11) years; and 38% on glucocorticoid therapy with ≥ 7.5 mg/day prednisone equivalent. The mean PSS score in the high stress group was 9.6 (± 1.9), compared with 3.5 (± 2.2) among the rest of the cohort. In the multivariate regression model, high stress was not associated with the Type 1 symptoms (worse scores for physician-assessed disease activity). However, high stress was associated with worse scores for each type 2 symptom: greater self-reported disease activity, lower cognitive function, more pain, and more fatigue (Table).
Conclusion: In a racially diverse sample of patients with SLE, high psychological stress was independently associated with worse type 2 symptoms including self-reported disease activity, cognitive dysfunction, pain, and fatigue. Evidence-based non-pharmacologic interventions to bolster stress resiliency, such as cognitive behavioral therapy, mindfulness-based stress reduction, and modified physical activity programs may be a strategy for improving outcomes in this patient population.
ACR2019_abstract_Table_CLUES_PSS_PRO_SLE
To cite this abstract in AMA style:
Patterson S, Trupin L, Lanata C, Murphy L, Hartogenesis W, Dall'Era M, Yazdany J, Katz P. Perceived Stress Independently Associates with Worse Type 2 Symptoms in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/perceived-stress-independently-associates-with-worse-type-2-symptoms-in-systemic-lupus-erythematosus/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/perceived-stress-independently-associates-with-worse-type-2-symptoms-in-systemic-lupus-erythematosus/
