Session Information
Date: Sunday, November 13, 2022
Title: SLE – Diagnosis, Manifestations, and Outcomes Poster II: Manifestations
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Long-term glucocorticoid use can lead to adverse outcomes independent of SLE disease activity. Identifying factors associated with long-term glucocorticoids is an important step towards better understanding the mechanisms by which patients remain on long-term glucocorticoids despite the availability of steroid sparing therapies. We sought to characterize the healthcare use of patients with SLE on long-term moderate to high dose glucocorticoid therapy.
Methods: We utilized an SLE registry at a large academic institution to compare acute care and outpatient resource utilization over one year among participants on long-term, moderate to high dose glucocorticoids. SLE was defined by either SLICC or ACR/EULAR criteria. Variables collected in the registry include, but are not limited to, age, sex, race, income, SLE medications, hospitalizations due to SLE, and SLE disease activity index 2000 (SLEDAI-2K). In the year prior to a participant’s first recorded SLEDAI-2K, we reviewed the medical record for emergency department visits and outpatient visits stratified by specialty and inclusion of ≥1 SLE-related diagnosis code. Long-term glucocorticoid use and typical dose were adjudicated in the medical record. Tapers and intravenous glucocorticoids were not considered long-term use. We defined high acute care utilization as ≥2 emergency department visits in the past year and moderate to high dose glucocorticoid use as a daily oral dose of >10 mg. Multivariable logistic regression of glucocorticoid use and high acute care use was performed, adjusting for SLEDAI-2K, hospitalization related to SLE, ≤3 SLE-related outpatient visits, and annual income < $25,000.
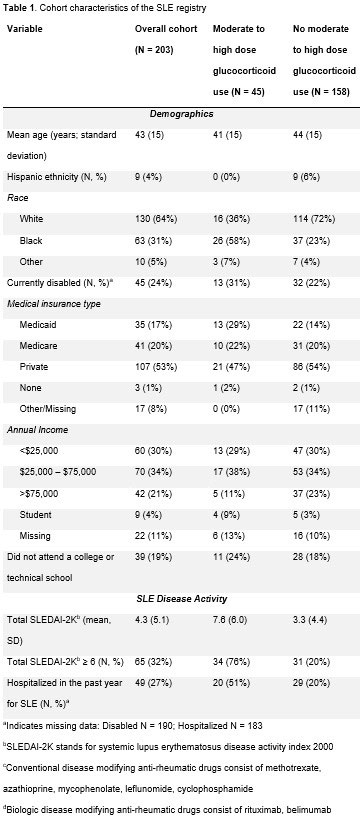
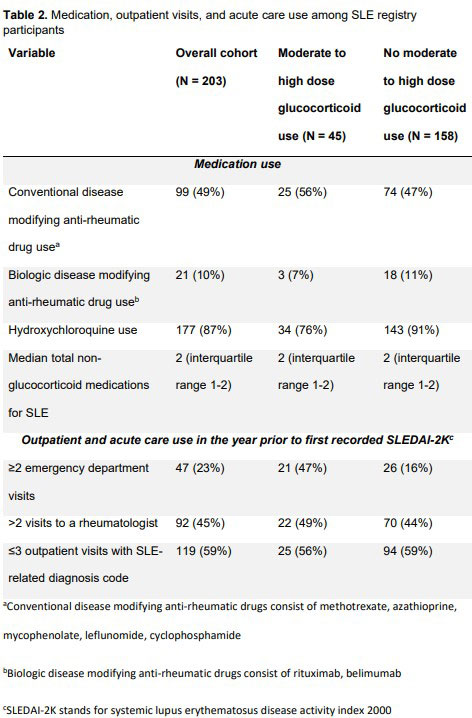
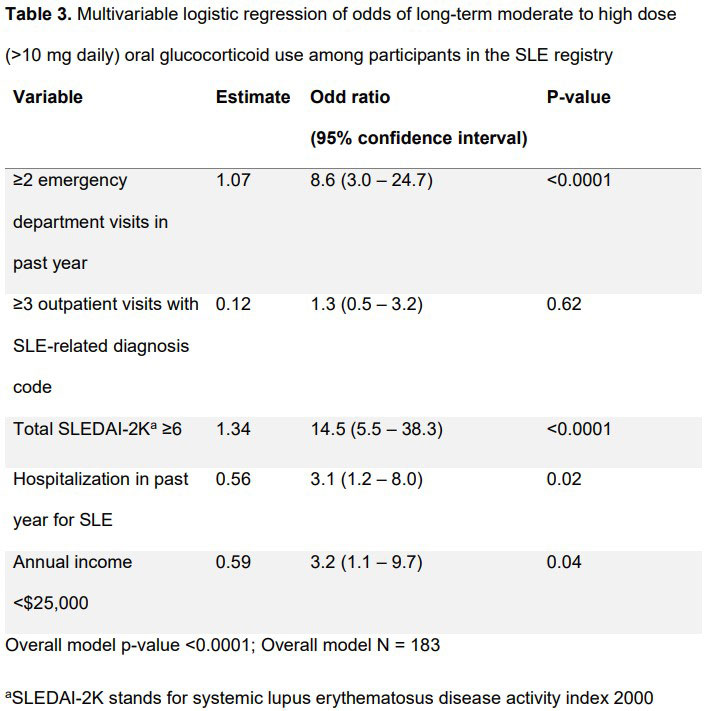
Results: Table 1 lists characteristics of the final 203 participant sample. A total of 100 participants were on long-term glucocorticoids, 55 of which were on 1-10 mg daily and 45 were on >10 mg daily. Among those not on glucocorticoids, 15% had ≥2 emergency department visits while 19% and 47% of those taking 1-10mg and >10mg daily had ≥2 emergency department visits, respectively. Medication, outpatient visits, and acute care use are listed in Table 2. In unadjusted analyses, moderate to high dose glucocorticoid use was associated with ≥2 emergency department visits in the past year (OR 4.4; 95%CI 2.2-9.1) and SLEDAI-2K ≥6 (OR 12.7; 95%CI 5.8-27.8), but not >2 rheumatologist visits or ≤3 SLE-related outpatient visits in the past year. The multivariable logistic regression model results are listed in Table 3. After adjusting for covariates, participants with high acute care utilization were more than 8-fold more likely to use long-term moderate to high dose glucocorticoids (adjusted OR 8.6; 95% CI 3.0-24.7; p< 0.0001, Table 2).
Conclusion: After adjusting for disease activity, annual income, hospitalization in the past year, and SLE-related outpatient visits, patients with SLE and high acute care use were more likely to use long-term moderate to high dose glucocorticoids. The reason for this association is likely multifactorial and warrants further exploration. Future research should examine the precise causes of this finding and future intervention should aim to increase the use of steroid sparing medications in this population.
To cite this abstract in AMA style:
Sullivan J, Littlejohn E. Patterns of Outpatient and Acute Care Use Among Patients with SLE on Long-Term Moderate to High Dose Glucocorticoid Medication: A 1 Year Retrospective Analysis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/patterns-of-outpatient-and-acute-care-use-among-patients-with-sle-on-long-term-moderate-to-high-dose-glucocorticoid-medication-a-1-year-retrospective-analysis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patterns-of-outpatient-and-acute-care-use-among-patients-with-sle-on-long-term-moderate-to-high-dose-glucocorticoid-medication-a-1-year-retrospective-analysis/