Session Information
Session Type: ARP Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Youth with child-onset systemic lupus erythematosus (SLE) transitioning from pediatric to adult health care systems may be at higher risk for poor outcomes than children or older adults with SLE. We leveraged US private insurance claims to describe patterns of ambulatory subspecialty care in transition-age youth with SLE, and to compare health care use and medication adherence before and after transfer to adult care. We hypothesized that ambulatory follow-up care and medication adherence decrease during the transfer period with a concurrent increase in acute care use.
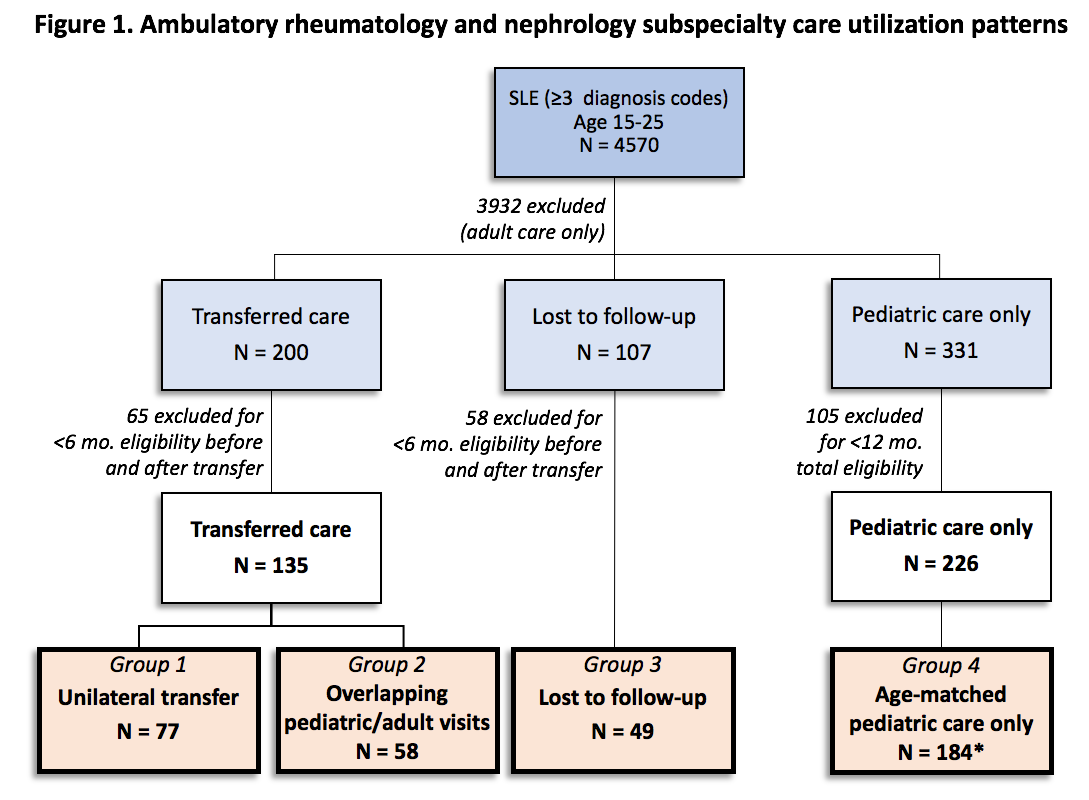
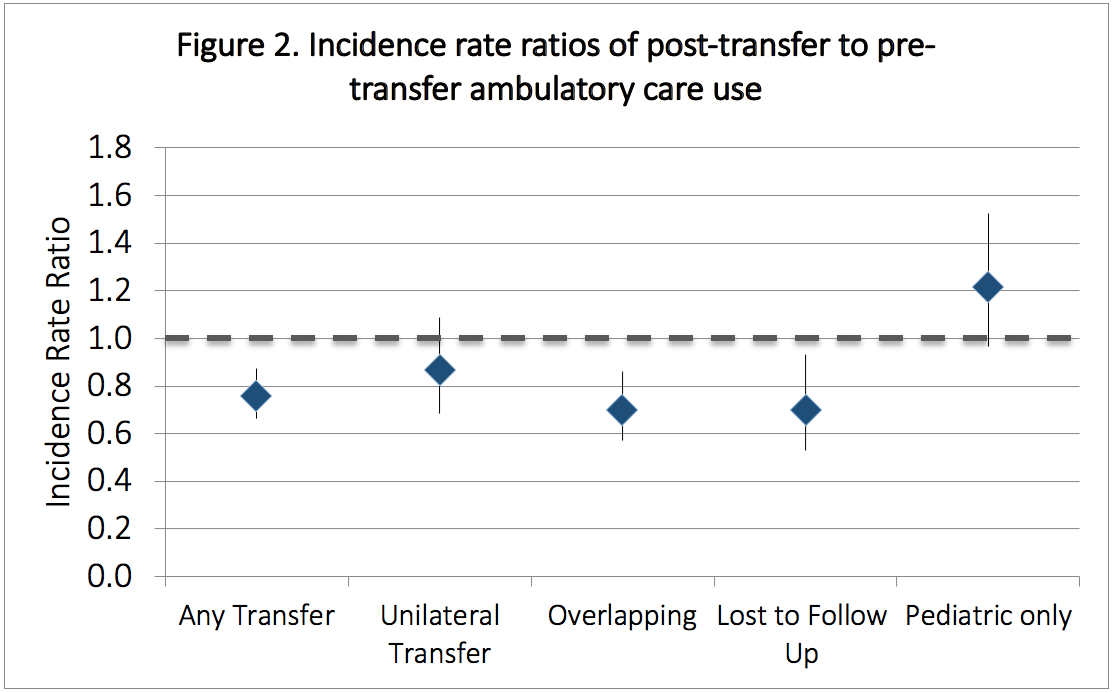
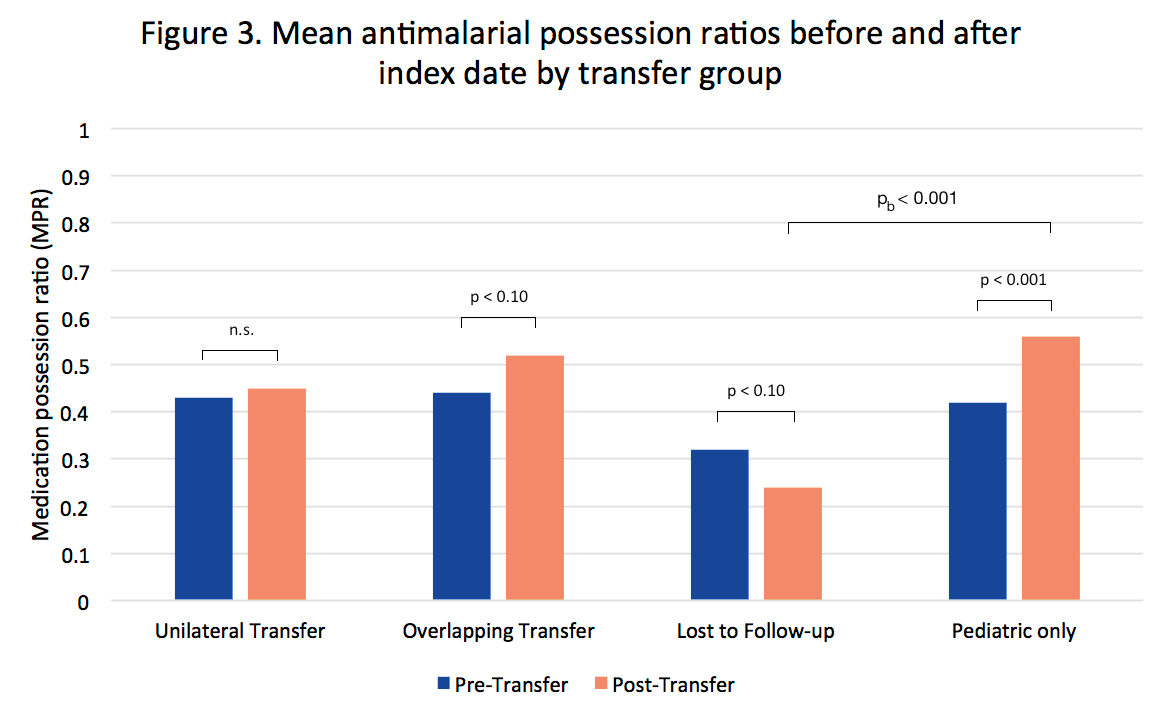
Methods: Using Clinformatics DataMart® (OptumInsight, Eden Prairie, MN) de-identified US claims data (2000-2016), we categorized youth ages 15-25 yrs with SLE by pattern of rheumatology/nephrology ambulatory care into those that 1) transferred unilaterally to adult care within 1 yr of the last pediatric visit, 2) had overlapping pediatric and adult visits before remaining in adult care 3) were lost to follow-up ( > 1 yr between last pediatric and first adult visit or end of enrollment), or 4) remained in pediatric care (Fig 1). The transfer index date was defined as the last pediatric visit for groups 1-3. Pediatric-only youth were age-matched to the other groups. We used negative binomial regression to compare pre- and post-transfer health care utilization rates within groups. We used paired t-tests to compare pre-/post- antimalarial medication possession ratios (MPR) in prevalent users, and compared MPRs between youth in groups 1-3 and their pediatric-only matches.
Results: A total of 184 youth with SLE met inclusion criteria for transfer out of pediatric rheumatology/nephrology care, of which 77 (42%) transferred unilaterally to adult care within a year, 58 (32%) had overlapping pediatric/adult care over a median of 12 months (IQR 4 – 27) before the last pediatric visit, and 49 (27%) were lost to follow-up. Of the 226 youth remaining in pediatric care, 107 were age-matched to each transfer group. Unilateral transfers were older than the lost to follow-up group (mean age 19.4 vs. 18.5, p 0.02) and more likely to live in the Northeast (p 0.04). Rates of ambulatory visits decreased after transfer among those with overlapping care and loss to follow-up, but remained unchanged among unilateral transfers (Fig 2). Rates of acute care utilization decreased across all groups (IRRs 0.14-0.30, p< 0.01). Average pre-transfer antimalarial MPRs ranged from 0.3-0.5 (Fig 3). Post-transfer MPRs were lower in the lost to follow-up group compared to age-matched peers remaining in pediatric care (mean 0.2 vs. 0.6, p< 0.01).
Conclusion: Among transition-age youth with SLE who have continuous private insurance coverage, acute care utilization does not increase during transfer to adult care. However, a substantial proportion of youth fail to see an adult provider within 12 months of the last pediatric visit. These youth have decreased rates of ambulatory care use and medication adherence compared to the pre-transfer period, and may be at highest risk for inadequate follow-up and poor outcomes. Additional data is needed to determine whether transfer patterns are associated with longitudinal health outcomes.
Funded by NIAMS, CARRA & the Arthritis Foundation.
To cite this abstract in AMA style:
Chang J, Knight A, Lawson E. Patterns of Ambulatory Health Care Utilization and Medication Adherence Among Transition-Age Youth with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/patterns-of-ambulatory-health-care-utilization-and-medication-adherence-among-transition-age-youth-with-systemic-lupus-erythematosus/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patterns-of-ambulatory-health-care-utilization-and-medication-adherence-among-transition-age-youth-with-systemic-lupus-erythematosus/