Session Information
Date: Monday, November 13, 2023
Title: (1155–1182) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: During the COVID-19 pandemic, there were growing concerns regarding the impact of SARS-CoV-2 on not only patients with rheumatic diseases but also the national hospital system. Research from prior studies on rheumatic and musculoskeletal diseases have identified higher rates of COVID-19 infection and higher mortality rate on a global scale; however, there is scant information on the economic burden on patients and the hospital system. In our study, we aim to analyze the demographic trend and inpatient hospital impact in the United States among patients admitted with concomitant COVID-19 infection and polymyositis.
Methods: We used the National Inpatient Sample (NIS), which is the largest public inpatient database of community hospitals, from 2020 and extracted adult patients (age 18 years and older) with the principal diagnosis of COVID-19 and secondary diagnosis of polymyositis based on the International Classification Disease version 10 (ICD-10) codes. All diagnoses were weighted to be nationally representative. Demographic characteristics, length of stay, hospitalization cost, and co-morbidities were analyzed using STATA, version 17. Pearson chi-squared test was used to compare categorical variables and studentt-test was used to compare continuous variables. Multivariable logistic regression was used to compare mortality with p-value set at < 0.05 for statistical significance.
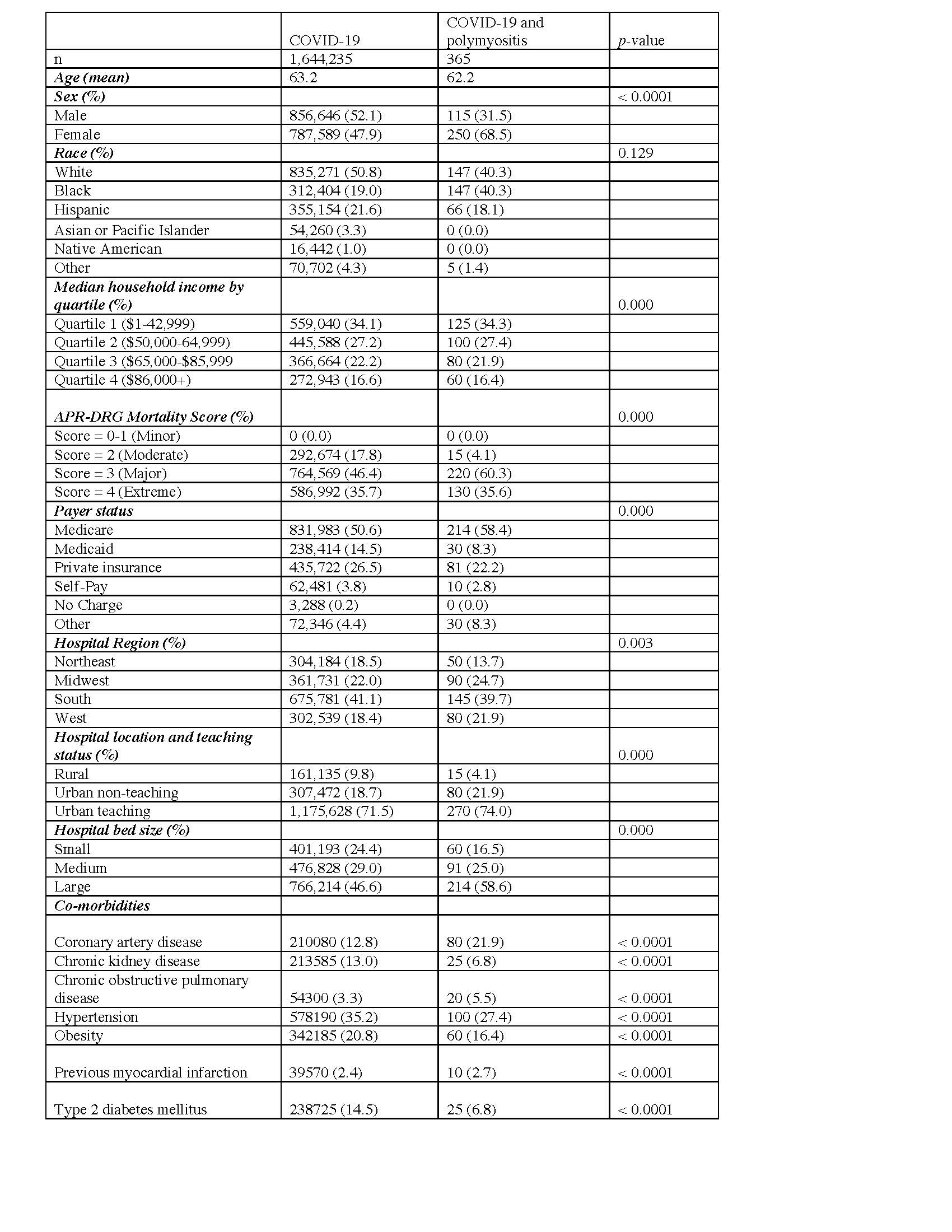
Results: 32,355,827 hospitalizations were included in the NIS 2020 database and 1,644,600 patients met our inclusion criteria. 365 patients with COVD-19 and polymyositis were admitted in 2020. Patients with COVID-19 as a primary diagnosis and polymyositis as a secondary diagnosis had a 1.98 times higher mortality than those with a diagnosis of COVID-19 alone (OR: 1.98, 95% CI: 1.15-3.42, p=0.01). COVID-19 cohort had average age of 63 years and 52.1% male compared to COVID-19 and polymyositis cohort who had average age of 62 years and 68.5% female. For COVID-19 patients, they were predominantly White, average hospital stay of 8days,and hospital cost $91,446. For COVID-19 and polymyositis cohort, they had a greater percentage of Black patients, predominantly female, average hospital stay of 8 days, and hospital cost $106,700. For co-morbidities, COVID-19 and polymyositis patients had a higher percentage of coronary artery disease and previous myocardial infarction (Table 1).
Conclusion: Both cohorts were predominantly treated at large teaching hospitals, approximate mean age of 60 years old, and over half of each cohort had hospital cost greater than their median household income. Despite these similarities between both groups, patients with pre-existing diagnosis of polymyositis with concomitant COVID-19 infection had almost double the inpatient mortality compared to patients who were hospitalized for COVID-19 alone. Our study highlights the importance of targeting at-risk patient demographics, particularly Black women who were more likely to be hospitalized for concomitant polymyositis and COVID-19 infection. This study not only augments prior research on inflammatory myopathy and COVID-19 infection, but also underlines the increased mortality risk and hospital cost in the American population.
To cite this abstract in AMA style:
He E, Sandhu V. Patients with COVID-19 and Polymyositis Inpatient Outcomes and Hospital Cost: Nationwide Inpatient Sample 2020 [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/patients-with-covid-19-and-polymyositis-inpatient-outcomes-and-hospital-cost-nationwide-inpatient-sample-2020/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patients-with-covid-19-and-polymyositis-inpatient-outcomes-and-hospital-cost-nationwide-inpatient-sample-2020/