Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose:
Due to improved mortality and morbidity in systemic lupus erythematosus (SLE), non-clinical indicators and outcomes, especially patient-reported ones, have become increasingly important in disease management in the past decades. The objective of our study was to identify dedicated standardized instruments (Patient-reported outcome measures; PROMS) for non-clinical indicators currently in use, and to demonstrate their relevance via their utilization by Lupus experts.
Methods:
To identify relevant non-clinical indicators, a systematic literature search was performed using the PubMed database in January 2018. In addition, guidelines, recommendations, consensus reports on the management and monitoring of SLE-patients as well as selected review articles on quality of life, disease burden, and patient-reported outcome were screened. Subsequently, a literature search was conducted for each of the non-clinical indicators to identify all dedicated patient-reported questionnaires in use. A questionnaire for SLE experts was compiled on the basis of the results obtained, covering the utilization of non-clinical indicators, their specific questionnaires and possible obstacles. The questionnaire was distributed to members of the European Lupus Society (SLEuro), as well as other Lupologists.
Results:
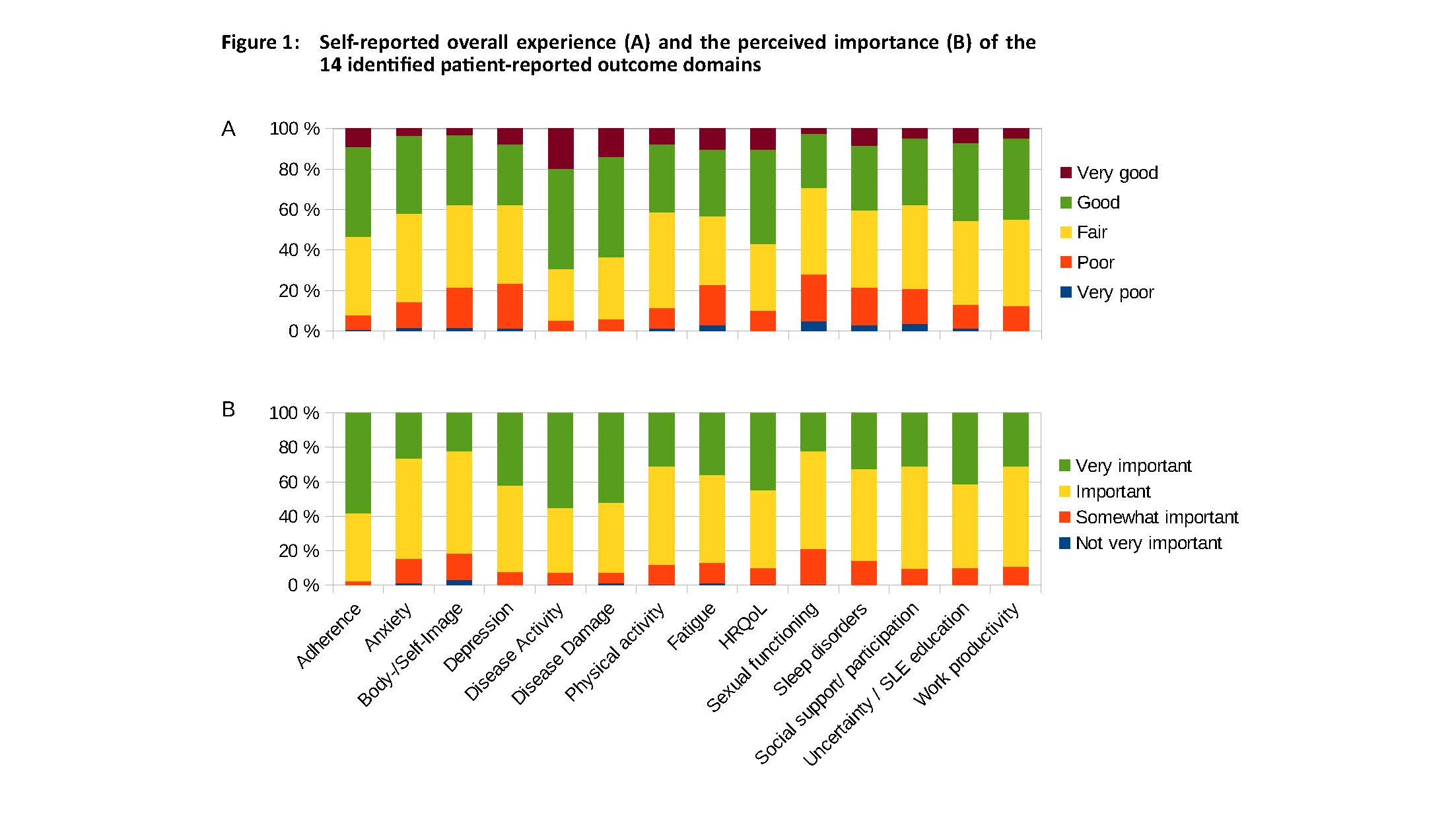
A total of 21 non-clinical indicators were identified, 7 of which did not have a standardized questionnaire. For the remaining 14 non-clinical indicators, 50 different questionnaires were found. 167 lupus experts from 43 countries participated in our study, of whom 57% stated to be members of a regional or national reference center for SLE. 73% claimed to treat more than 30 and 37% more than 90 SLE-patients per year (see table 1). Self-reported overall experience and the perceived importance of the 14 identified patient-reported outcome domains by the lupus experts are shown in figure 1. 31% reported to use PROMS to monitor disease outcome in their lupus patients, e.g. for assessing (health-related) quality of life (22.9%) or fatigue (15.7%). The top 5 reasons for not using PROMS were ‘Lack of time’ 87%, ‘Lack of linguistically validated questionnaires’ 32%, ‘Lack of validated questionnaires’ 28%, ‘Discordance with my assessment/impression’ 15%, and ‘Poor credibility of the results’ 12%.
Conclusion:
Despite the increasing importance of PROMS received for regulatory studies in recent years, their use has not yet become established in routine use among lupus experts. Although numerous PROMS on different endpoints are available, they are relatively rarely used in everyday clinical practice nor for clinical decision-making. Better availability of validated multilingual instruments and better incentives (proven benefit for care, additional remuneration) could contribute to improved utilization.
Acknowledgement: This project received funding from the European Commission under the 3rd Health Programme, grant agreement No PP-2-4-2016.
To cite this abstract in AMA style:
Chehab G, Richter J, Kernder A, Tani C, Lorenzoni V, Elefante E, Palla I, Cannizzo S, Pirri S, Triulzi I, Trieste L, Turchetti G, Mosca M, Schneider M. Patient-reported Outcome Measures in Systemic Lupus Erythematosus: Use in Clinical Practice – Preliminary Results from the Integrate Project [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/patient-reported-outcome-measures-in-systemic-lupus-erythematosus-use-in-clinical-practice-preliminary-results-from-the-integrate-project/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patient-reported-outcome-measures-in-systemic-lupus-erythematosus-use-in-clinical-practice-preliminary-results-from-the-integrate-project/