Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic Lupus Erythematosus is characterized by diverse clinical presentations and a remarkably unpredictable course. Although survival rate has increased in recent decades, morbidity and mortality are still substantially high, resulting in multiple hospital admissions. Winning the battle against lupus requires a good understanding of the causes of SLE-related hospital admissions and the predictors of morbidity and mortality, in order to implement the early necessary interventions to reduce poor outcomes in hospitalized patients. Because SLE disease course, prognosis, and management vary across races and countries, understanding these factors in different populations is highly important.
Methods: Electronic records of SLE patients admitted to Hamad General Hospital over a period of 3 years were reviewed to obtain patients’ demographics, clinical characteristics and hospitalization outcomes, and identify predictors of intensive care unit (ICU) admission and poor outcomes. All analyses were performed using Stata 17. Continuous variables were summarized as medians and interquartile ranges; categorical variables as frequencies and percentages. Group comparisons used chi-square tests for categorical and Wilcoxon tests for continuous variables. Logistic regression analyzed binary outcomes (ICU admission), and multivariable regression adjusted for confounders, presenting adjusted odds ratios with 95% confidence intervals. Statistical significance was defined as a p-value < 0.05.
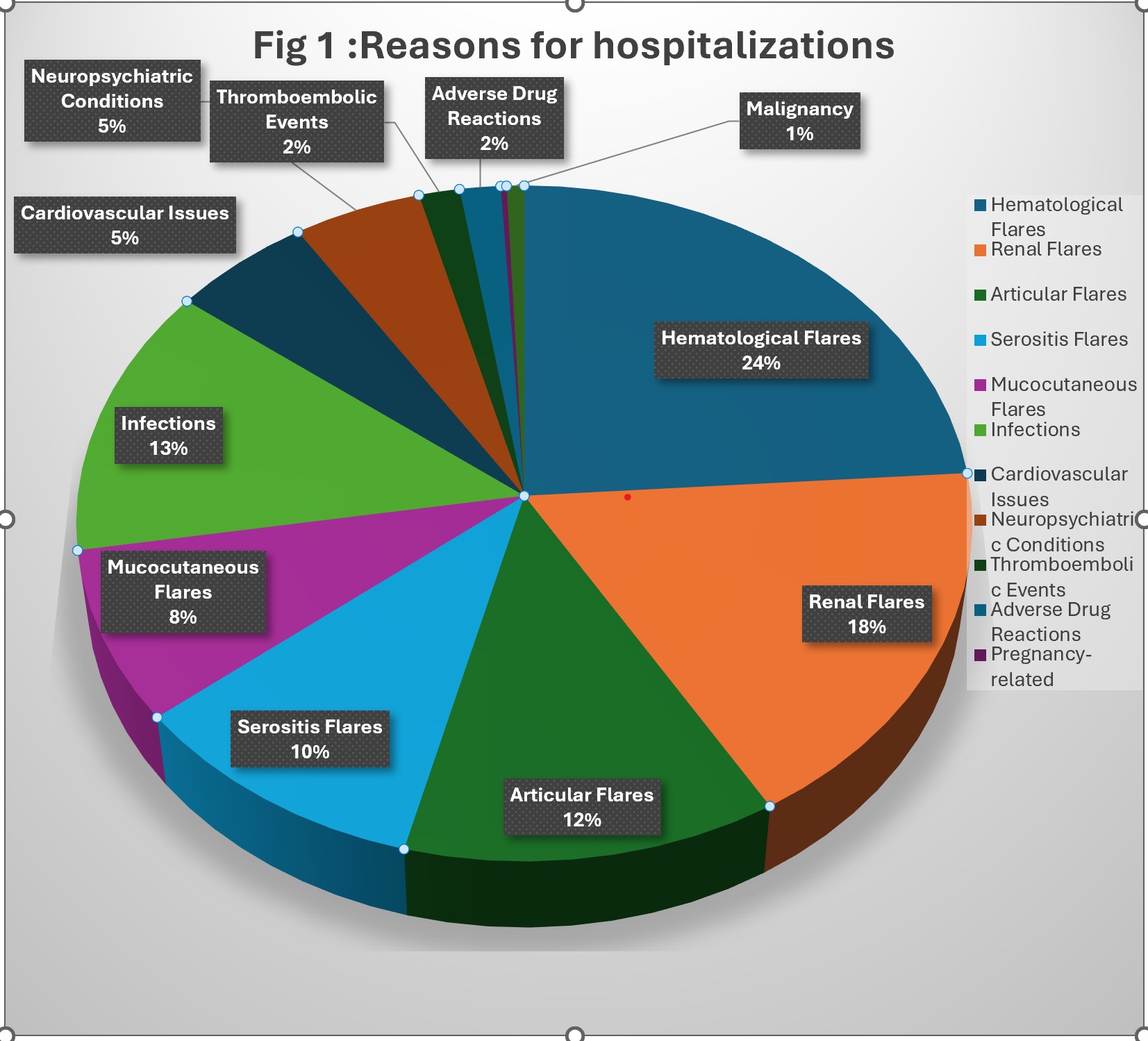
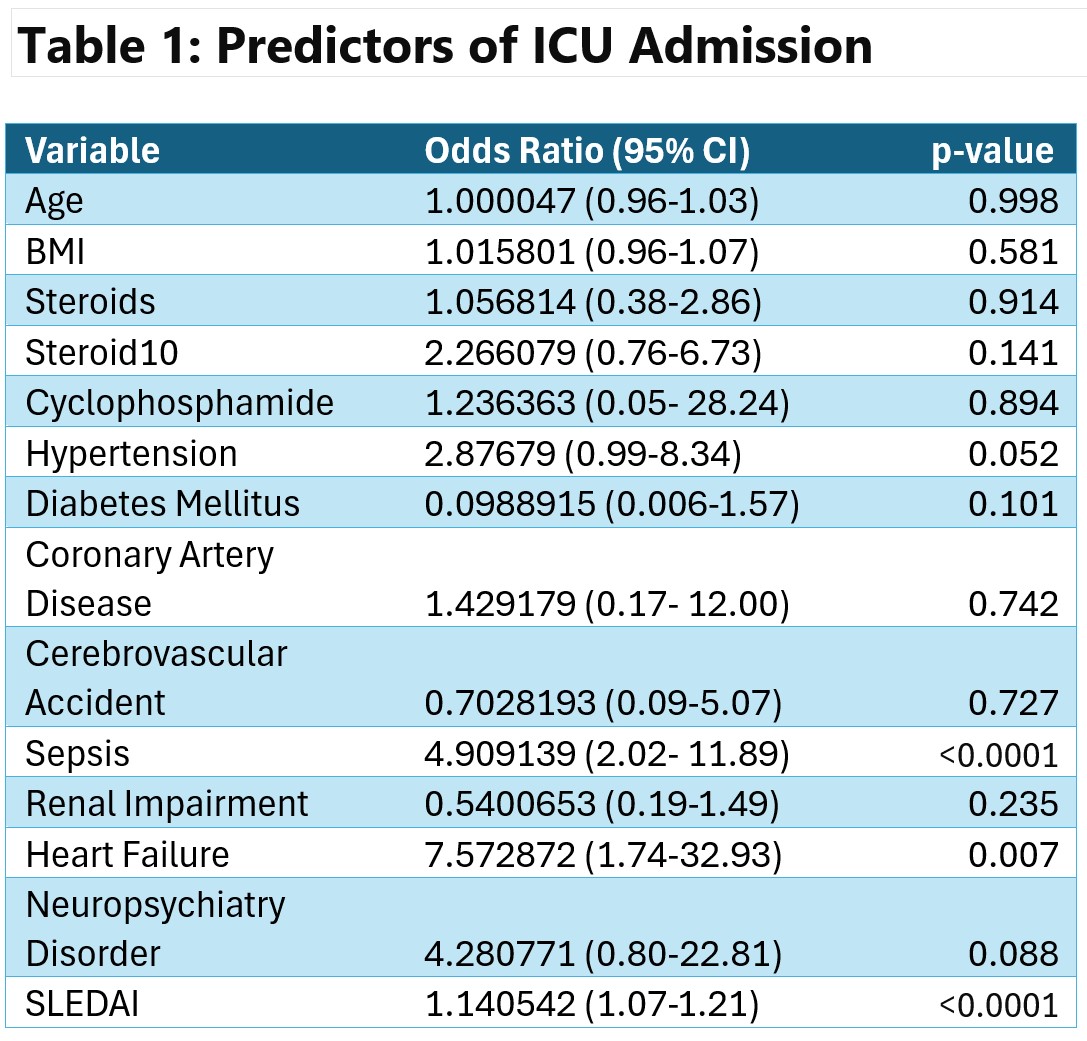
Results: A total of 280 admissions for 153 patients were analyzed. The median age was 34 years (IQR: 26-45), with 90% female, 28% from the Gulf, and 24% Southeast Asian. 80% had a known diagnosis with a median age of 27 years (IQR: 21-36) and a median disease duration of 5 years (IQR: 1-10). Renal involvement in 38% and antiphospholipid syndrome in 18%. Hypertension was the main comorbidity in 33%. The primary reasons for hospital admission were disease flares (hematological 38%, renal 28%) and infections (20%) (fig 1). The median SLEDAI score was 7 (IQR: 3-12). 56% were on hydroxychloroquine and 51% on steroids, with 20% on doses ≥10 mg prednisolone. The median hospitalization length was 7 days (IQR: 4-12) with 51% having ≥2 admissions. Major complications included renal impairment (40%) and sepsis (23%). There were 46 ICU admissions with a median stay of 7 days (IQR: 3-15). Sepsis, heart failure, higher SLEDAI score, and steroid doses >10 mg were associated with ICU admission (Table 1). 5 deaths (1.8%) occurred, mainly due to septic shock.
Conclusion: In this multinational cohort, sepsis, cardiovascular complications, high disease activity, and high steroid doses were associated with poor outcomes. Optimizing disease control, preventing infections, and managing comorbidities can improve hospitalization outcomes. Although the proportion of ICU admissions was substantially high, mortality remained relatively low, reflecting the quality of care. These findings will aid in predicting poor outcomes and implementing early interventions to reduce morbidity and mortality.
To cite this abstract in AMA style:
Gharib M, Becetti K, J.Abukhadijah H, Alam F, Padmakumari A, Awni AlKahlout M, sheikh saleh r, Bilal Jamshaid M, Alemadi S. Outcomes of Systemic Lupus Erythematosus Hospitalizations: Insights from a Multinational Tertiary Center Experience [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/outcomes-of-systemic-lupus-erythematosus-hospitalizations-insights-from-a-multinational-tertiary-center-experience/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/outcomes-of-systemic-lupus-erythematosus-hospitalizations-insights-from-a-multinational-tertiary-center-experience/