Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Osteoporosis is associated with increased morbidity and mortality. There is a 60% risk of a subsequent fracture for patients who have had one fracture, with vertebral compression fractures having the highest rate of recurrent fragility fracture, and hip fractures being the most common recurrent fracture type at 3 years. Fracture Liaison Services (FLS) are secondary fracture prevention systems that channel hospital-admitted patients to an osteoporosis clinic that have been shown to lower recurrent fracture rates. An FLS at our institution addresses care gaps; a local study showed that up to 90% of fracture patients are never offered screening or treatment for osteoporosis by their primary care physician (PCP). The purpose of this study is to determine the effectiveness of the FLS by analyzing outcome measures related to initiation of treatment, DXA utilization and risk factor assessment.
Methods: Hospital admission data extraction from our Epic® electronic health record (EHR) was done using ICD 10 codes on fragility fracture for pre-FLS data (September 2015-March 2017) and post-FLS (September 2017-February 2019). Chart review was done to retrieve the following data: patient demographics (age, sex, ethnicity), body mass index, weight, height, circumstances of fracture (fragility vs traumatic), anatomic location, prior fractures, primary care provider location, treatment initiation, calcium and vitamin D supplementation, and laboratory data (TSH, PTH, 25-OH-Vitamin D). A 10% improvement in outcome measures related to treatment initiation and DXA utilization were previously set. Percent improvement in these measures, including p-values were calculated, and barriers to care were identified.
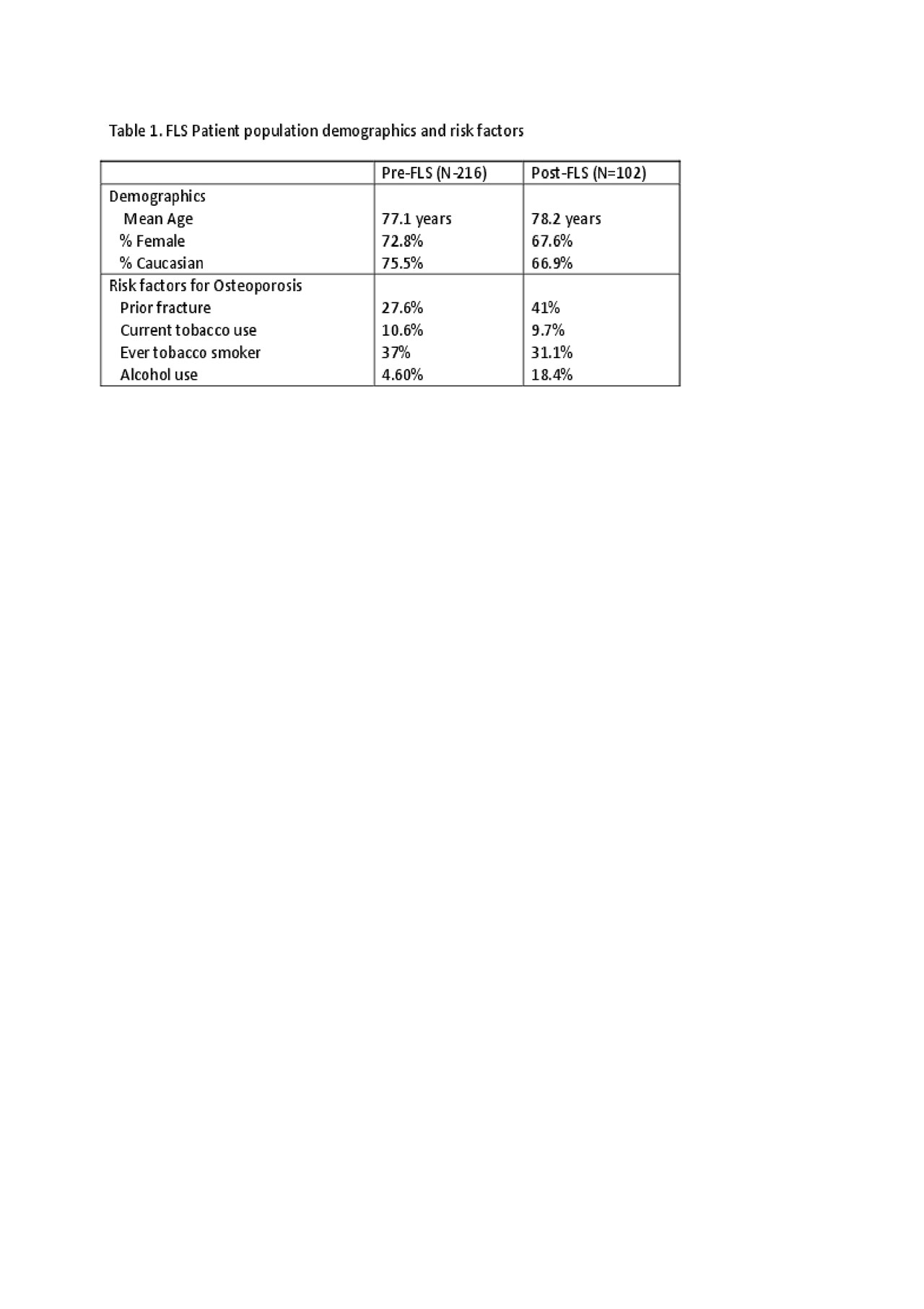
Results: Patient demographics, medication initiation, calcium and vitamin D supplementation and risk factor assessment between pre- and post-FLS groups were noted. (Table 1 and 2) Patient populations pre and post-FLS were similar. Overall, a 10% improvement in outcome measures were met except for pharmacotherapy initiation and DXA scan post-fracture. The barrier to medication initiation was most commonly due to reluctance of patients to take medications for prevention of further fractures which typically stems from inability to understand the risk of side effects as compared to the risk of a subsequent fracture.
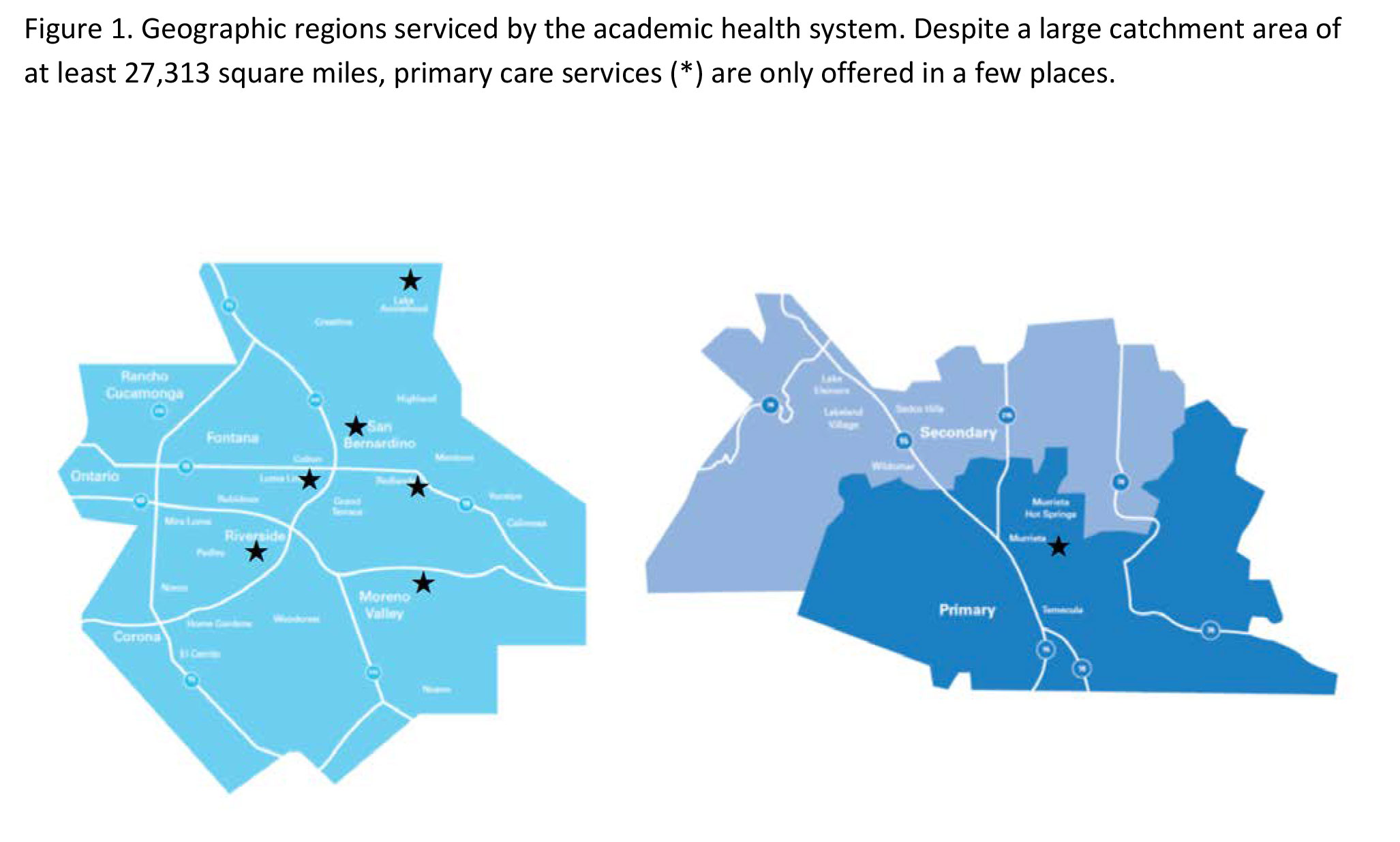
Out of 92 FLS referrals inpatient, only 27 (29.3%) were adherent with osteoporosis clinic visits. Many patients admitted to the academic medical center are referred from other centers and have outside PCPs, and at an institutional level, primary care services are limited. (Figure 1) A Primary Care Institute was established 2018. It is hoped this would increase patient adherence to visits.
Conclusion: The Fracture Liaison Service met targeted improvements in outcomes in calcium and vitamin D supplementation but not in DXA post-fracture or pharmacotherapy initiation. Improving risk communication physician skills, while necessary, also need to consider patient perspectives on treatment recommendations. Improving access to local Primary Care can improve adherence to osteoporosis specialty clinic visits. Tracking re-fracture events in these patients is also needed.
To cite this abstract in AMA style:
Yu M, Jose D, Hudson P, Downey, MD C, Phipatanakul W, Giannelli S, Codorniz K, Torralba K. Outcomes of a Fracture Liaison Service at an Academic Health Center [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/outcomes-of-a-fracture-liaison-service-at-an-academic-health-center/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/outcomes-of-a-fracture-liaison-service-at-an-academic-health-center/