Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Many effective medications are available for osteoporosis treatment. However how rheumatologists use these therapies is not well understood, particularly in patients with concomitant rheumatologic conditions. The objective of this study was to examine the patterns of utilization of osteoporosis medications among rheumatologists reporting to the ACR’s Rheumatology Informatics System for Effectiveness registry (RISE).
Methods: RISE is a national registry that passively collects data from real-world rheumatology practices. As of December 2018, RISE held validated data from 715 rheumatology providers in 226 practices, representing ~20% of the U.S. clinical rheumatology workforce. Patients included in this study were ≥18 years old and had osteoporosis based on ≥ 1 diagnosis code for osteoporosis or prescriptions/administrations of osteoporosis medications, each calendar year from 2015 to 2018. We identified autoimmune rheumatic disease type using ICD10 codes. We assessed osteoprosis medication use, including bisphosphonates, denosumab, and anabolics in each calendar year from 2015 to 2018, examining both prevalent use (i.e. any use) and separately, new osteoporosis medication initiation (i.e. use in that year, with no prior recorded use in RISE in any previous year).
Results: In 2018, we identified 251,620 eligible patients from 217 practices. Of these, 89.6% were female, 68.4% were white, 4.5% were black, and 7.5% were identified as Hispanic or Latino with an overall mean age of 73.0 +/- 11.3 years. The most common co-morbid autoimmune rheumatic disease in this cohort was RA (11.9%). The underlying rheumatic disease by first line osteoporosis medication choice is presented in the table. In 2018, a nominally greater proportion (18.5%) of patients initiated denosumab, compared to bisphosphonate therapy (16.9%). Of patients who initiated denosumab in 2018, 34.6% had a prior recorded history of being on bisphosphonate therapy. Conversely, 9.0% of patients that started bisphosphonates in 2018 had a prior recorded history of being on denosumab previously. In patients who had never received any osteoporosis therapy, bisphosphonates remained the most frequently prescribed first-line treatment in 2018. Using the same definition of osteoporosis, compared to prior years, we observed a decline in proportion of registry participants initiating osteoporosis medications in each calendar year, decreasing from 47.9% in 2015 to 42.1% in 2016, 40.5% in 2017, and 36.5% in 2018, despite an increasing number of patients in the registry with osteoporosis (Figure).
Conclusion: Osteoporosis medication initiation in rheumatology practices declined over 2015-2018, however denosumab treatment appears to be gaining popularity. Bisphosphonate therapy remains favored as first line therapy for osteoporosis, but overall denosumab was initiated more frequently in 2018 compared to bisphosphonate therapy or anabolics.
(Disclaimer: This data was supported by the ACR’s RISE Registry. However, the views expressed represent those of the authors, not necessarily those of the ACR)
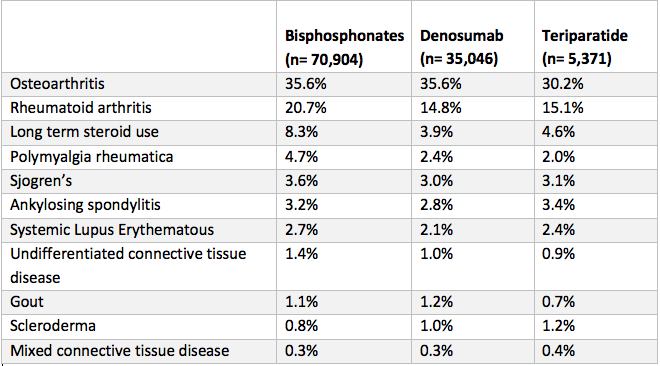 Osteoporosis therapy initiated by U.S. rheumatologists participating in RISE in 2018 by patients’ underlying rheumatologic diagnosis.
Osteoporosis therapy initiated by U.S. rheumatologists participating in RISE in 2018 by patients’ underlying rheumatologic diagnosis.
To cite this abstract in AMA style:
Khullar N, Chen L, Curtis J, Baker J, Yun H, Reimold A, Danila M. Osteoporosis Medication Utilization Patterns over Time in the ACR RISE Registry [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/osteoporosis-medication-utilization-patterns-over-time-in-the-acr-rise-registry/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/osteoporosis-medication-utilization-patterns-over-time-in-the-acr-rise-registry/

