Session Information
Title: Rheumatoid Arthritis - Clinical Aspects (ACR): Comorbidities, Treatment Outcomes and Mortality
Session Type: Abstract Submissions (ACR)
Background/Purpose:
It is recommended that a joint be classified as clinically swollen if this swelling is beyond doubt. However in clinical practice the evaluation of joint swelling in patients with rheumatoid arthritis (RA) is often hindered by joint deformity, secondary osteoarthritis (OA) or adiposity. The aim of this study was to evaluate the ambiguity and reliability of clinical swollen joint assessment in patients with RA.
Methods:
Clinical joint swelling was evaluated in 2 cohorts of consecutive RA patients with at least 1 swollen joint. In Cohort A (n=20) a conventional 28 swollen joint count (SJC) was performed on the same day by 2 independent, blinded examiners. In Cohort B (n=28) the same examiners performed a modified 28 SJC in which joints were graded as either definitely swollen, non-swollen or doubtfully swollen (defined as a joint where swelling can not be excluded or confirmed due to limited evaluation attributed to the physical characteristics of the joint). In addition a standard grey-scale (GS) and Power Doppler (PD) ultrasonographic evaluation (US) was performed by a sonographer blinded to clinical data in Cohort B patients. Presence/absence of GS synovitis, PD signal, erosion and osteophytes were recorded.
Results:
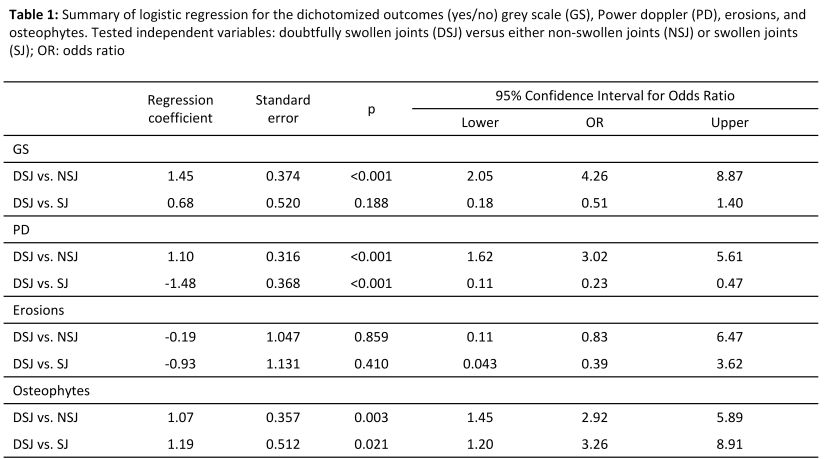
A total of 1316 joints were clinically evaluated in 48 RA patients (89% women; mean(±): age: 59.4 (12.1) years, disease duration: 12.5 (8.1) years, SDAI: 10.74 (8.9)) in 2 cohorts. Eighty-five percent (24 out of 28) of patients in Cohort B had at least 1 doubtfully swollen joint, with a maximum number of 4 doubtful joints/patient. The top joints with doubtful swelling were the wrist, knee, MCP3 and MCP1 joint. Interobserver reliability, evaluated by intraclass correlation coefficient in Cohort A for the conventional SJC and in Cohort B for the modified SJC was 0.80 (95% confidence interval (95%CI) 0.77-0.83) and 0.83 (95%CI: 0.81-0.85) respectively. Agreement between the 2 examiners for definitely swollen and doubtfully swollen joints was 65% and 16% respectively. Doubtfully swollen joints were more often GS (p<0.001) and PD positive (p<0.001) as compared to non-swollen joints (80% vs. 54% and 26% vs. 12% respectively) and had more frequently osteophytes on US than either swollen (p=0.021) or non-swollen joints (p=0.003) (11% vs. 4.5/4.5% respectively). Erosions were more commonly detected in swollen joints than in doubtfully swollen or non-swollen joints (4.8% vs. 1.8/2.2%) (Table 1). No association was found between body mass index and the number of doubtfully swollen joints.
Conclusion:
A modified SJC including doubtfully swollen joints is characterized by similar interobserver reliability as the conventional SJC. Agreement between 2 blinded examiners was low for the evaluation of doubtful swelling. Doubtfully swollen joints had significantly more osteophytes on US suggesting a relationship between ambiguity of swelling and secondary OA in patients with RA.
Disclosure:
P. Mandl,
None;
P. Studenic,
None;
G. Supp,
None;
T. A. Stamm,
None;
M. Sadlonova,
None;
M. Ernst,
None;
S. Haider,
None;
D. Aletaha,
None;
J. Smolen,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/osteophytes-increase-the-ambiguity-of-clinical-evaluation-of-joint-swelling-in-rheumatoid-arthritis/