Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Recent studies in the general population highlight possible adverse cardiovascular effects with calcium supplementation; however, the association between calcium intake and subclinical markers of atherosclerosis has not been explored in patients with rheumatoid arthritis, a group with increased risk for coronary artery disease and cardiovascular mortality.
Methods: Among RA patients participating in a cohort study of subclinical cardiovascular disease (CVD), daily supplemental calcium dose was assessed from prescription and over the counter medications at baseline and at the first follow-up visit (median time from baseline 20 months). Participants underwent 64-slice cardiac multidetector row CT scanning at baseline and at visit 3 (median time 39 months from baseline) to assess coronary artery calcium (CAC), a measure of coronary atherosclerosis. The relationship of average daily intake of calcium (mg/day) with CAC was assessed by multivariable ordinary logistic regression with CAC score dichotomized at 100 units (a level predictive of subsequent CVD events), and adjusting for relevant confounders.
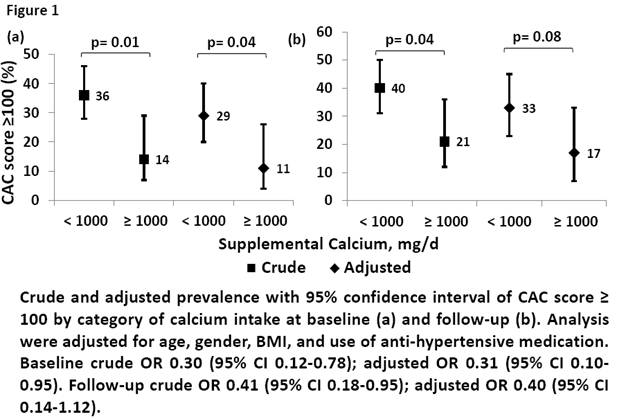
Results: A total of 145 RA patients [38% male, mean age 59±8 years, median RA duration 9 years, mean DAS28 3.6±1.0] had complete longitudinal data. At baseline, 42 (28%) were taking ≥1000mg/d of calcium while the remainder took <1000mg/d. A CAC score ≥100 units was observed in 44 (30%) at baseline and 51 (35%) at follow-up. Age, gender, body mass index (BMI), and use of anti-hypertensives were associated with both CAC and calcium intake, and were considered as relevant confounders in subsequent analyses. At baseline, CAC scores of ≥100 were significantly less frequent in the higher vs. lower dose calcium supplementation groups [OR 0.30 (95% CI 0.12-0.78) (Fig 1a)], and this difference remained significant after adjustment for relevant confounders [OR 0.31 (95% CI 0.97-0.95) (Fig 1a)]. Similarly, at follow-up, CAC scores of ≥100 were also significantly less frequent in the group taking an average calcium supplement dose of ≥1000mg/d vs. those taking <1000mg/d (Fig 1b); however, when adjusted for relevant confounders, there was only a trend to significance [OR 0.40 (95% CI 0.14-1.15) (Fig 1b)]. There was no gender heterogeneity in the association of calcium intake with CAC score. Change in CAC score over time between baseline and follow-up was not statistically significantly different between the two calcium groups.
Conclusion: Calcium supplementation was not associated with a higher risk of coronary atherosclerosis in this RA population, and may have even been protective, a finding with relevant therapeutic implications in the daily treatment of RA patients.
Disclosure:
S. Dhaduvai,
None;
L. Geraldino-Pardilla,
None;
J. T. Giles,
None;
J. M. Bathon,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/oral-calcium-supplementation-is-associated-with-subclinical-atherosclerosis-in-rheumatoid-arthritis/