Session Information
Date: Wednesday, October 24, 2018
Title: 6W027 ACR/ARHP Abstract: Health Services Research II: Economic & Clinical Implications (2994–2999)
Session Type: ACR/ARHP Combined Abstract Session
Session Time: 11:00AM-12:30PM
Background/Purpose: SLE patients frequently experience pain. Opioid use for the management of chronic pain has been associated with increased morbidity, mortality, and healthcare resource utilization. We investigated the prevalence and factors associated with opioid use among MILES Cohort participants to identify opportunities to improve quality of care in SLE.
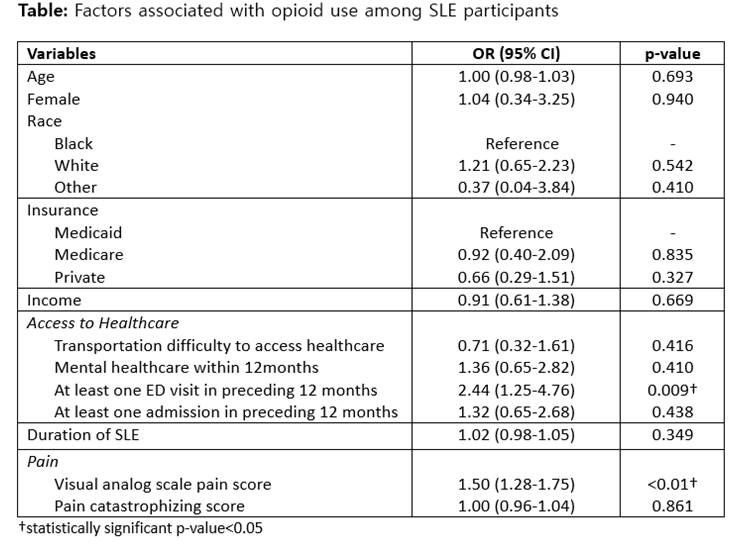
Methods: Data were derived from structured interviews at baseline visit of MILES, a longitudinal, population-based cohort of 462 SLE participants and 192 controls matched across sex, age, race and geography in southeastern Michigan. Detailed information on opioid use including prescribed frequency (scheduled or as needed) and duration were obtained. For the 30 SLE participants who reported more than one opioid use, opioid with longest duration was included in the analyses. We used multivariable logistic regression to evaluate factors associated with opioid use among SLE participants. Variables determined a priori to be important, or with p-values <0.1 in univariate analysis, were included in multivariable models (see Table).
Results: All 654 participants completed the MILES Cohort baseline visit; average age 53.4 (SD 12.8), 584 (89%) female, 288 (44%) black and 159 (24%) with Medicaid insurance. Only 15 controls (8%) reported opioid use compared to 143 among SLE participants (31%) (p<0.001). One in three controls were prescribed scheduled opioids, whereas half of the SLE participants on opioids were given scheduled prescriptions. SLE participants on average reported 6 years of opioid use (SD 7 years) compared to 3 years among controls (SD 2 years) (p=0.140). Moreover, 34% of SLE participants on opioids reported opioid usage ≥5 years, whereas only 7% of controls on opioids had usage ≥5 years (p=0.037) (see Figure). In multivariable analysis, among SLE participants, those with higher pain score [OR 1.50 (95% CI 1.28-1.75)] and at least one ED visit in the preceding 12 months [2.43 (1.25-4.74)] were more likely to be on opioids (see Table).
Conclusion: One in three SLE participants reported opioid use, and a third of those have opioid usage ≥5 years. Higher pain score and having at least one ED visit were significantly associated with opioid use. Studies have shown patients who frequent the ED are more likely to be prescribed opioids for pain. Moreover, opioid prescription in the ED has been found to increase the risk of long-term opioid therapy and associated morbidity and mortality. Further study is warranted to improve pain management and reduce opioid use in SLE participants, particularly for those who frequent the ED, to improve quality of care.
To cite this abstract in AMA style:
Lee J, Padda A, Marder W, Harlow S, Hassett AL, Zick S, Helmick CG, Barbour KE, Gordon C, Minhas D, McCune WJ, Somers EC. Opioid Use Among SLE Patients and Controls in the Population-Based Michigan Lupus Epidemiology & Surveillance (MILES) Cohort [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/opioid-use-among-sle-patients-and-controls-in-the-population-based-michigan-lupus-epidemiology-surveillance-miles-cohort/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/opioid-use-among-sle-patients-and-controls-in-the-population-based-michigan-lupus-epidemiology-surveillance-miles-cohort/