Session Information
Date: Sunday, November 8, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Comorbidities
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: One in four Medicare hospitalizations with systemic lupus erythematosus (SLE) results in readmission within 30 days, with “injuries and poisonings” as the second most common cause. This finding, which could be driven by opioid use, coupled with a recent study reporting that as many as 31% of patients with lupus received at least one opioid prescription in a year (Sommers 2019), raised new questions as to whether a focus on opioids could inform mechanistic-focused readmission reduction strategies. To begin to test the strength of this premise, we examined the extent to which prior opioid-related encounters in the baseline year predicted risk for 30-day readmission.
Methods: One in four Medicare hospitalizations with systemic lupus erythematosus (SLE) results in readmission within 30 days, with “injuries and poisonings” as the second most common cause. This finding, which could be driven by opioid use, coupled with a recent study reporting that as many as 31% of patients with lupus received at least one opioid prescription in a year (Sommers 2019), raised new questions as to whether a focus on opioids could inform mechanistic-focused readmission reduction strategies. To begin to test the strength of this premise, we examined the extent to which prior opioid-related encounters in the baseline year predicted risk for 30-day readmission.
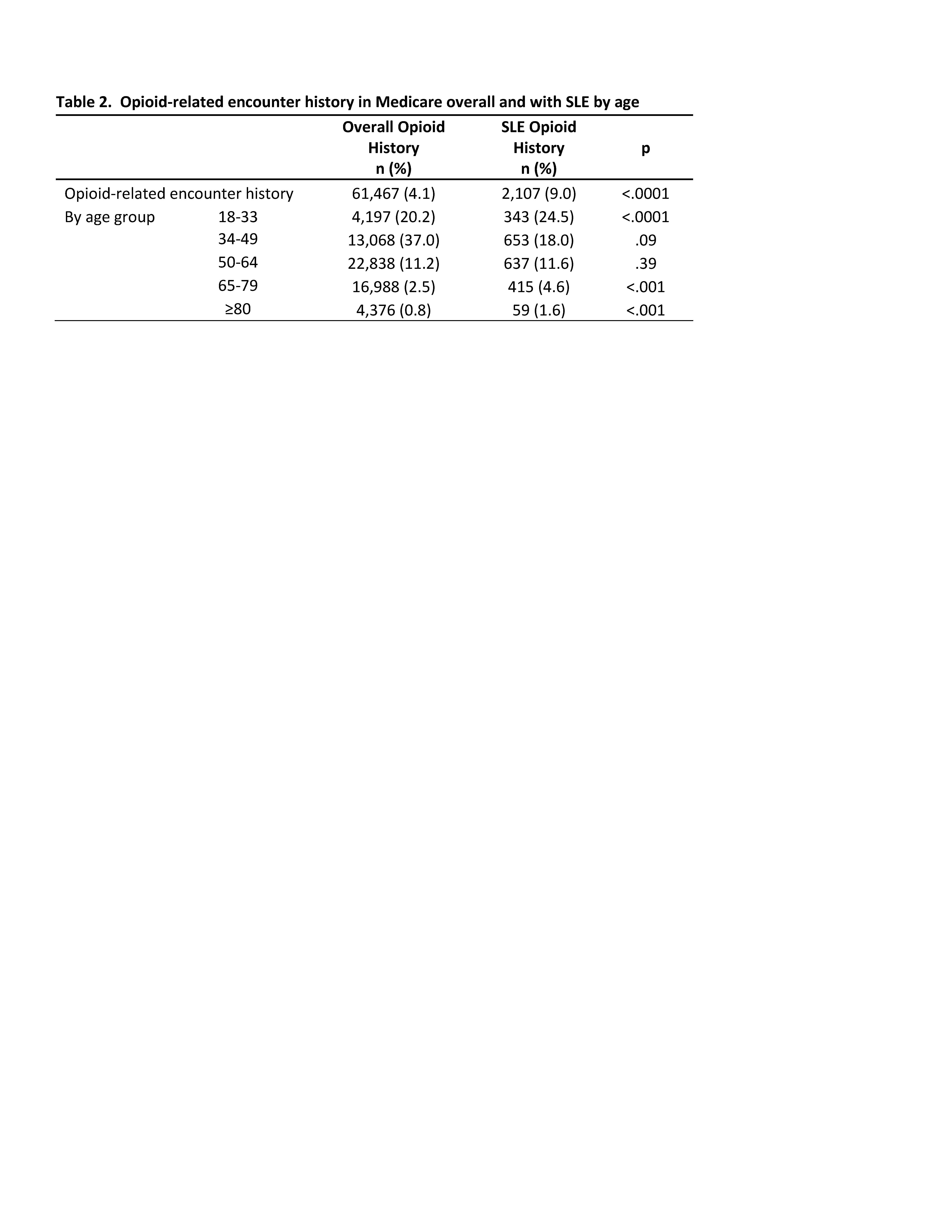
Results: Table 1 shows that compared to the overall Medicare admissions cohort, the SLE cohort (n=23,309) was younger, and more often female, Black, disabled or on Medicaid, or had end stage renal disease (ESRD). In SLE, those with prior opioid-related codes were younger and more often female or receiving Medicaid or disability. Readmissions occurred in 18% of overall Medicare and 24% of SLE admissions. In SLE, observed readmission rates were 10% higher among those with opioid history (33% vs 23%, p< .001). The SLE group was over twice as likely as the overall Medicare group to have had opioid-related encounters in the prior year (9.0% vs 4.1%, p< .001; Table 2). Opioid-related codes were highest in the youngest SLE group; 25% of admissions of 18-32 year olds had prior opioid-related encounters (vs. 20% in Medicare cohort, p< .001).
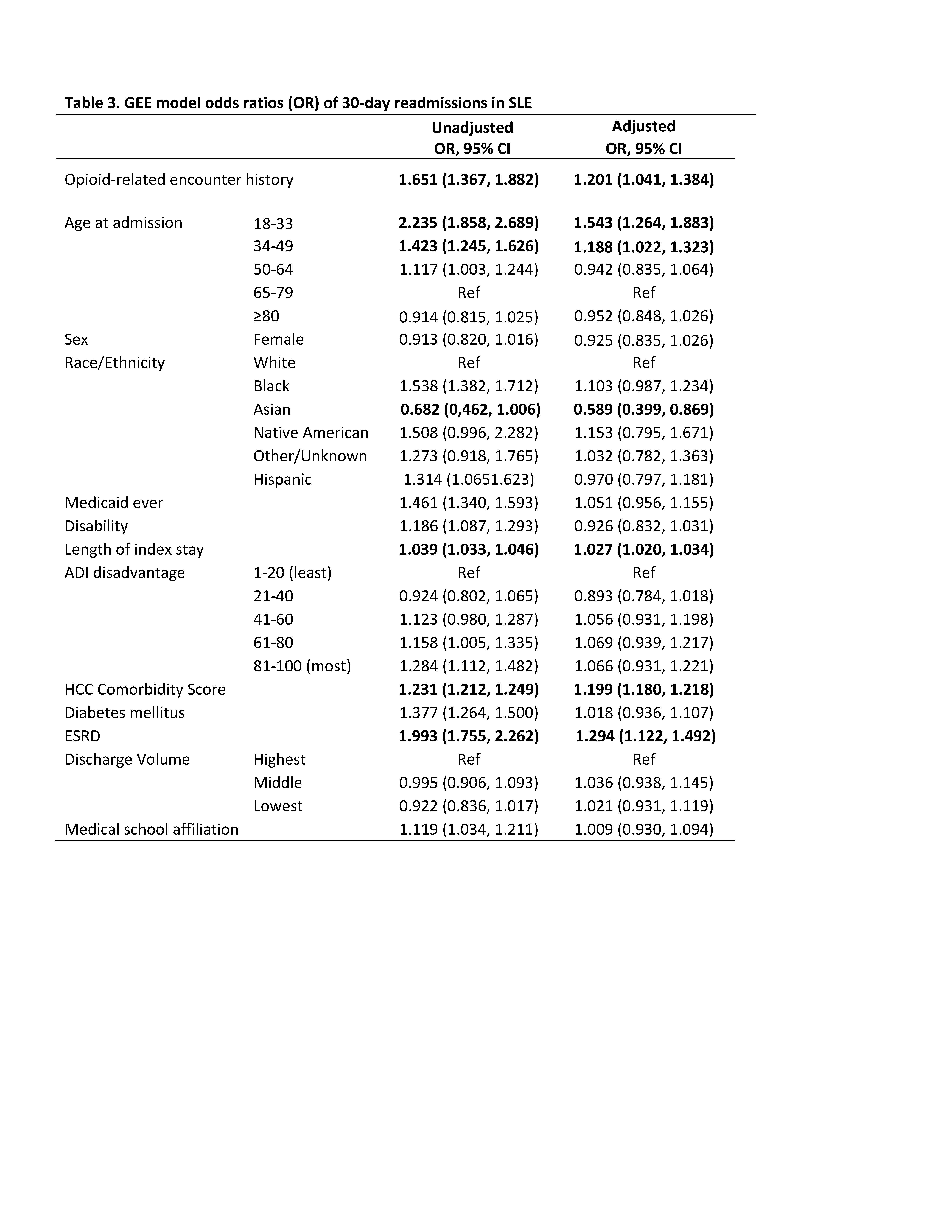
Adjusted multivariable models showed 20% higher odds of readmission (aOR 1.201 (1.041, 1.384)) with opioid history (Table 3). This was similar in magnitude to an increase in composite comorbidity (HCC aOR 1.199 (1.180, 1.218)), and slightly less than ESRD (ESRD aOR 1.294 (1.122, 1.491)).
Limitations include the absence of Medicare Part D pharmacy claims to further examine opioid history, thus rates may not reflect actual opioid use.
Conclusion: Hospitalized Medicare beneficiaries with SLE were twice as likely to have prior opioid-related encounters, and exposure to these opioid-related encounters was associated with a substantially increased readmission risk even after adjusting for comorbidities. Future studies should investigate readmission reduction interventions to help SLE patients with opioid histories.
To cite this abstract in AMA style:
Bartels C, Schletzbaum M, Chen Y, Kind A. Opioid-Related Encounters as a Predictor of 30-Day Readmissions in Lupus [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/opioid-related-encounters-as-a-predictor-of-30-day-readmissions-in-lupus/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/opioid-related-encounters-as-a-predictor-of-30-day-readmissions-in-lupus/