Session Information
Date: Tuesday, November 12, 2019
Title: Epidemiology & Public Health Poster III: OA, Gout, & Other Diseases
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatic diseases can be associated with pain and disability. An international opioid epidemic is ongoing, and prescription opioid use has been linked with increased risks of addiction, abuse, and mortality. We assessed contemporary opioid prescription patterns among patients with rheumatic diseases in a general population context.
Methods: Using a United Kingdom general population database, we identified cohorts of fibromyalgia, chronic inflammatory arthritis (including RA, ankylosing spondylitis [AS], and psoriatic arthritis [PsA]), systemic autoimmune rheumatic diseases (SARDs) (including SLE, Sjogren’s syndrome, systemic sclerosis, dermatomyositis, polymyositis, mixed connective tissue disease, ANCA-vasculitis, and Bechet’s disease), and gout by Read codes and examined opioid prescriptions between January 1, 2000 and December 31, 2016 within these cohorts. We estimated the annual prevalence of opioid prescriptions among prevalent cases in each disease cohort. We also estimated the annual incidence of new opioid prescriptions among incident patients in each disease cohort, as determined by the percentage who received an opioid prescription within one year following their diagnosis and were free of opioid prescriptions in the antecedent 6 months. We examined secular trends by prescription opioid (e.g., tramadol, codeine) and strong opioids including morphine, oxycodone, fentanyl, hydromorphone, and methadone) within each disease cohort.
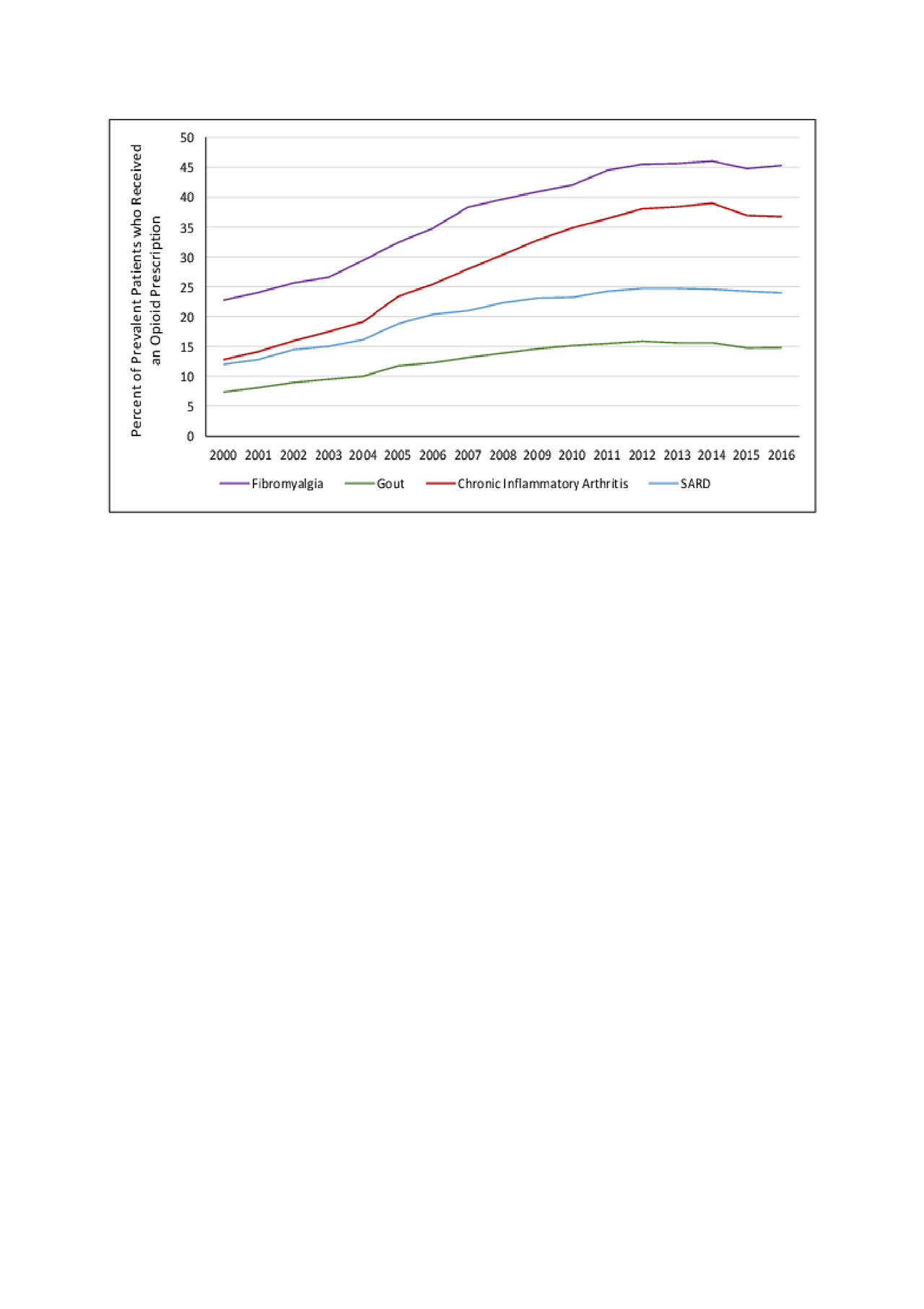
Results: Among incident cohorts, we identified 26,267 with fibromyalgia, 39,954 with inflammatory arthritis, 9,800 with SARDs, and 135,130 with gout. Prevalent opioid prescriptions increased in each disease cohort, reaching a plateau between 2012 and 2016 (Figure 1). In 2016, 45.2% of patients with fibromyalgia, 36.7% with inflammatory arthritis, 24.0% with SARD, and 14.8% with gout received opioid prescriptions. Tramadol was the most commonly prescribed individual opioid (19.4%, 13.0%, 8.7%, and 5.2% prevalence, respectively), whereas 20.1%, 15.2%, 10.1%, and 3.6% of patients received strong opioid prescriptions, respectively. Patients with fibromyalgia were the most likely to receive new opioid prescriptions; annual rates rose from 12.8% in 2000 to 22.6% in 2016 (Figure 2). This was followed by incident inflammatory arthritis and SARDs, and the annual incidence was lowest among gout patients, rising from 5.3% to 9.5%.
Conclusion: In this general population-based study, we identified a substantial rise in the rates of opioid prescriptions among patients with rheumatic disease. Between 2012 and 2016, nearly half of patients with fibromyalgia, over one-third of patients with RA, PsA, and AS and nearly one-fourth of patients with SARDs received opioid prescriptions. These findings highlight the importance of increased awareness, as this population may be at risk for opioid-related complications.
Systemic Autoimmune Rheumatic Disease -SARD- includes systemic lupus erythematosus, Sjogren’s syndrome, systemic sclerosis, dermatomyositis, polymyositis, mixed connective tissue disease, ANCA-associated vasculitis, and Behcet’s disease. Chronic inflammatory arthritis includes rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis.
Systemic Autoimmune Rheumatic Disease -SARD- includes systemic lupus erythematosus, Sjogren’s syndrome, systemic sclerosis, dermatomyositis, polymyositis, mixed connective tissue disease, ANCA-associated vasculitis, and Behcet’s disease. Chronic inflammatory arthritis includes rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis.
To cite this abstract in AMA style:
Jorge A, Lu N, Choi H. Opioid Prescription Use Among Patients with Rheumatic Disease: A Population Based Cohort Study [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/opioid-prescription-use-among-patients-with-rheumatic-disease-a-population-based-cohort-study/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/opioid-prescription-use-among-patients-with-rheumatic-disease-a-population-based-cohort-study/