Session Information
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: The chronic and recurrent nature of antiphospholipid syndrome (APS) leads to damage accrual that impairs long-term functional status and survival. The Damage Index for Antiphospholipid Syndrome (DIAPS) is a validated instrument designed to capture the damage accrual in thrombotic APS, but it is not known whether it correlates with mortality. We aim to determine whether early damage, as measured by the DIAPS, predicts long-term mortality in thrombotic APS.
Methods: We carried out a retrospective analysis of all medical records to calculate the yearly DIAPS score of 197 thrombotic APS patients attending the Rheumatology and/or Haematology clinics at a tertiary hospital for up to 43 (median 10) years. Patients fulfilled the 2006 Sydney classification criteria. The disease onset was the time the first thrombotic event related to APS was diagnosed. Early damage refers to damage present at six months after the disease onset. Early DIAPS increase refers to the increase of at least one point from the initial DIAPS score within the first five years after the disease onset. DIAPS score is shown as median (interquartile range, IQR). We used logistic, and uni and multivariable Cox regression models to analyse risk factors affecting mortality. Survival was analysed through the Kaplan-Meier method.
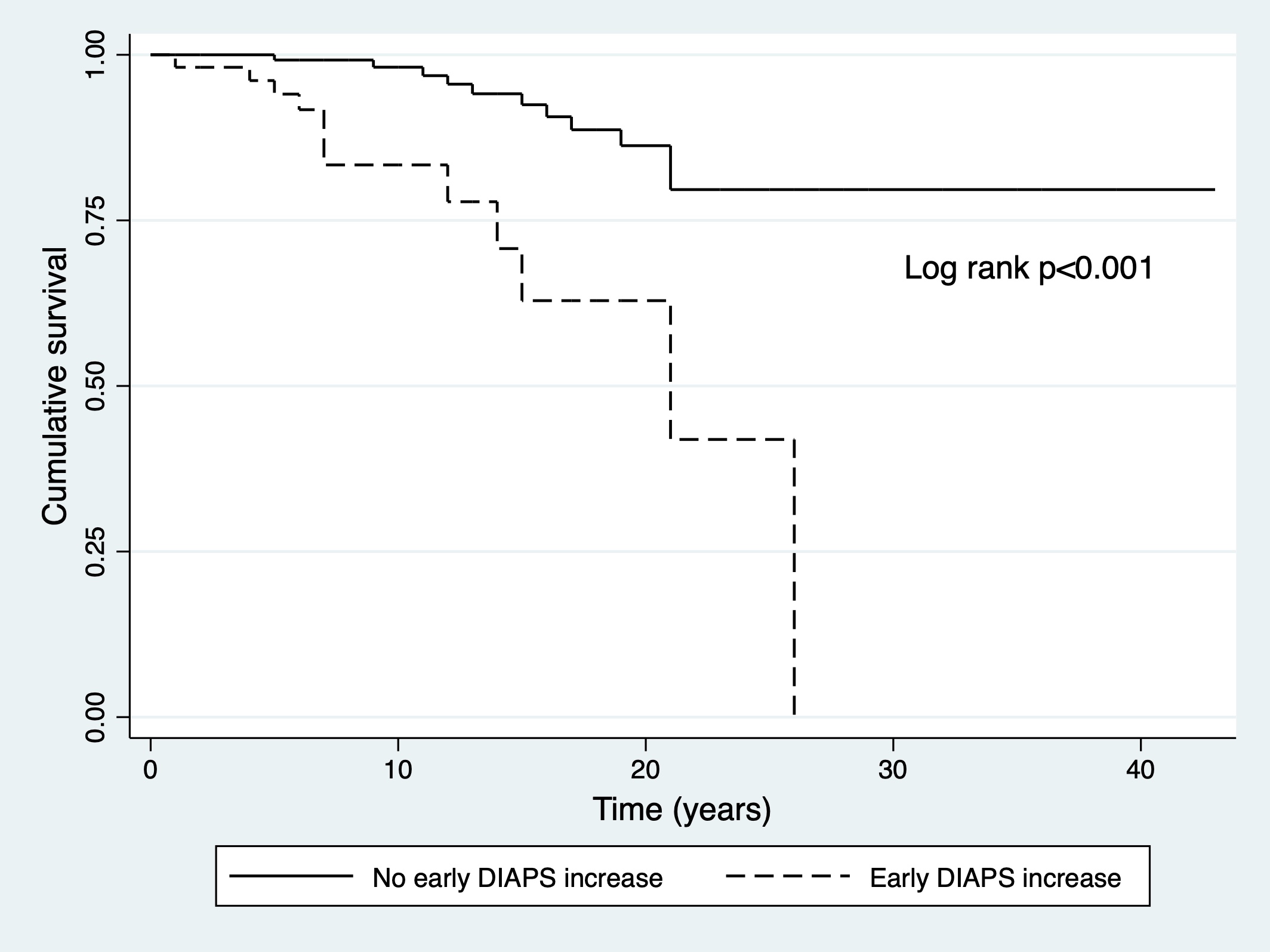
Results: The median age at APS onset was 40 (IQR 51-28) years, with a female (71%) and primary APS (66%) preponderance. Caucasian ethnicity was the most prevalent (72%), followed by Asian (10%), Afro-Caribbean (9%) and other (9%). Damage developed in 143 (73%) patients with a median DIAPS score of 1 (IQR 2-0) at the last visit. Early damage was present in 69 (35%) patients. Early DIAPS scored low values in the whole group (0, IQR 1-0). We identified 23 fatalities (12%). Patients who died had higher last DIAPS (2, IQR 3-1 vs. 1, IQR 2-0, p=0.012) but similar early DIAPS score (0, IQR 1-0 vs. 0, IQR 1-0, p=0.318) compared to those who survived. Secondary APS (HR 3.07, 95% CI 1.32-7.12, p=0.009), male gender (HR 3.14, 95% CI 1.35-7.33, p=0.008) and age at APS onset ≥40 years (HR 5.34, 95% CI 1.96-14.53, p=0.001) were risk factors for death. Early damage was not associated with death (HR 1.65, 95% CI 0.73-3.78, p=0.231). Conversely, early DIAPS increase, present in 29% (53/181) of patients, was associated with death (HR 5.40, 95% CI 2.33-12.52, p< 0.001), even after adjusting individually for APS category (secondary, HR 5.05, 95% CI 2.18-11.72, p< 0.001), gender (male, HR 5.40, 95% CI 2.29-12.73, p< 0.001) and age at APS onset (≥40 years, HR 3.41, 95% CI 1.43-8.20, p=0.006). Figure 1 shows the survival analysis. Having a first arterial thrombotic event was associated with early damage (OR 7.24, 95% CI 3.74-14.03, p< 0.001), but not with early DIAPS increase (OR 1.22, 95% CI 0.64-2.33, p=0.539) nor with the risk of death (HR 1.85, 95% CI 0.79-4.27, p=0.151).
Conclusion: These findings suggest that damage accrual accessed by DIAPS is associated with increased mortality in a large multi-ethnic group of APS patients. In particular, an increase of at least one point on DIAPS in the first five years after disease onset, but not early damage, is an important predictor of mortality regardless of the nature of the first thrombotic event, gender, APS category and age.
To cite this abstract in AMA style:
Gaspar P, Farinha F, Sayar Z, Efthymiou, M, Cohen H, Isenberg D. One Point Increase in the Initial Damage as Measured by the Damage Index for Antiphospholipid Syndrome Predicts Mortality in a Multi-Ethnic Group of Thrombotic Antiphospholipid Syndrome Patients [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/one-point-increase-in-the-initial-damage-as-measured-by-the-damage-index-for-antiphospholipid-syndrome-predicts-mortality-in-a-multi-ethnic-group-of-thrombotic-antiphospholipid-syndrome-patients/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/one-point-increase-in-the-initial-damage-as-measured-by-the-damage-index-for-antiphospholipid-syndrome-predicts-mortality-in-a-multi-ethnic-group-of-thrombotic-antiphospholipid-syndrome-patients/