Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Tapering of disease-modifying therapy (DMARDs) is recommended by EULAR/ACR for rheumatoid arthritis (RA) patients who achieve sustained remission on stable therapy. However, there is no guidance on how to manage this in clinical practice. We aimed to assess flare over 12 months in RA patients who were offered structured tapering of either conventional synthetic (cs) or biologic (b) DMARDs.
Methods:
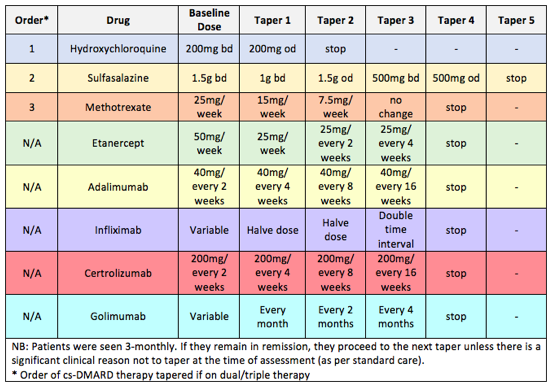
RA patients (ACR/EULAR 2010) prospectively attending a remission clinic were recruited when fulfilling the criteria of stable remission as defined by 3-variable DAS28<2.6 for >= 6 months (stable therapy & no corticosteroids). Patients were offered tapering according to a structured protocol (Figure 1). For patients receiving combination cs/b-DMARDs, only the b-DMARD was tapered. Clinical, ultrasound (US) + immunological (T-cell subsets: naive, Treg (both age-corrected) and inflammation related cells, IRC) data were collected. Flare over a period of 12 months was assessed using several definitions in order to evaluate their relevance for clinical outcomes. Associations with baseline characteristics were assessed using univariate statistics (Mann-Whitney-U and Chi-square). No correction for multiple testing was attempted.
Results:
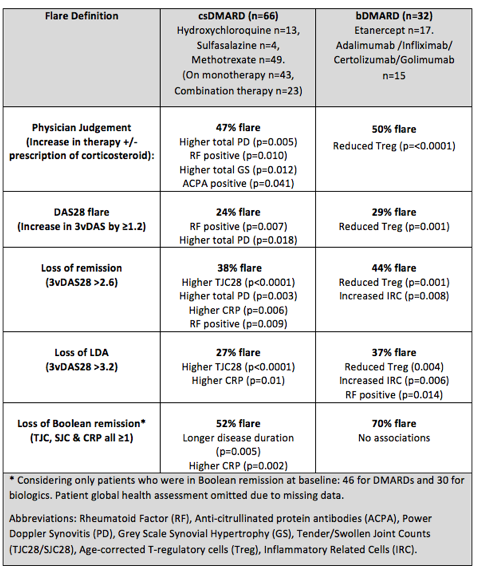
98 patients (cs-DMARDs n=66, b-DMARDs n=32) accepted tapering and achieved at least 12 months follow-up. In the cs-DMARD group 55% were female; the median age was 64 years and median remission duration 25 months. For b-DMARDs 63% were female; the median age was 61 years and median remission duration 28 months. There was great heterogeneity in terms of flare rate according to the definitions used (Table 1). Tapering of b-DMARDs was associated with higher flare rate (29-70%) compared to cs-DMARDs (24-52%). Demographics were not associated with flare by any definition (except longer disease duration for cs-DMARD patients who lost Boolean remission status). Clinical (notably seropositivity) and US measures were associated with flare for cs-DMARDs. Reduced Treg and higher IRCs at baseline were associated with flare in patients tapering b-DMARDs.
Conclusion:
The flare rate varied with the definition used and was more common when tapering b-DMARDs compared to cs-DMARDs. Flare was predicted in the latter patients by clinical and US (including seropositivity) findings, whereas T-cell abnormalities predicted flare in b-DMARD patients. These results will help formulate further tapering strategies.
Table 1. Rate of flare according to different definitions and associations with baseline characteristics
Figure 1. Tapering Protocol
To cite this abstract in AMA style:
Gul H, Ponchel F, Emery P. On Tapering Therapy for RA Patients in Clinical Remission; Flare on Csdmards Predicted By Clinical Features and Musculoskeletal Ultrasound, Whereas T-Cell Abnormalities Predictive for b-DMARD Tapering [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/on-tapering-therapy-for-ra-patients-in-clinical-remission-flare-on-csdmards-predicted-by-clinical-features-and-musculoskeletal-ultrasound-whereas-t-cell-abnormalities-predictive-for-b-dmard-tapering/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/on-tapering-therapy-for-ra-patients-in-clinical-remission-flare-on-csdmards-predicted-by-clinical-features-and-musculoskeletal-ultrasound-whereas-t-cell-abnormalities-predictive-for-b-dmard-tapering/