Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Reports in recent decades show drastic improvements in survival of SLE patients, with 10-15 year survival rates of >90%. However, little is known about North American Natives (NAN) with SLE. We compared mortality in NAN SLE patients to Caucasian (CA) SLE patients.
Methods: Patients from a single academic center were followed from 1990-2013 using a custom database. Variables included date of birth, diagnosis, age at disease onset, ethnicity, clinic visits dates, and vital status if known. Records of all patients with a diagnosis of SLE (≥4 American College of Rheumatology criteria) were abstracted. For patients who had not been seen in the last 2 years, updated vital status was obtained from the hospital medical records department. Ethnicity was by self-report, and categorized into NAN, CA and other. Age at diagnosis, disease duration and age at last follow up or age at death was calculated and compared between ethnic groups. Survival time was compared between NAN and CA using Kaplan Meier and Cox proportional hazard models, and person years of life lost (PYLL) was calculated for the 2 groups.
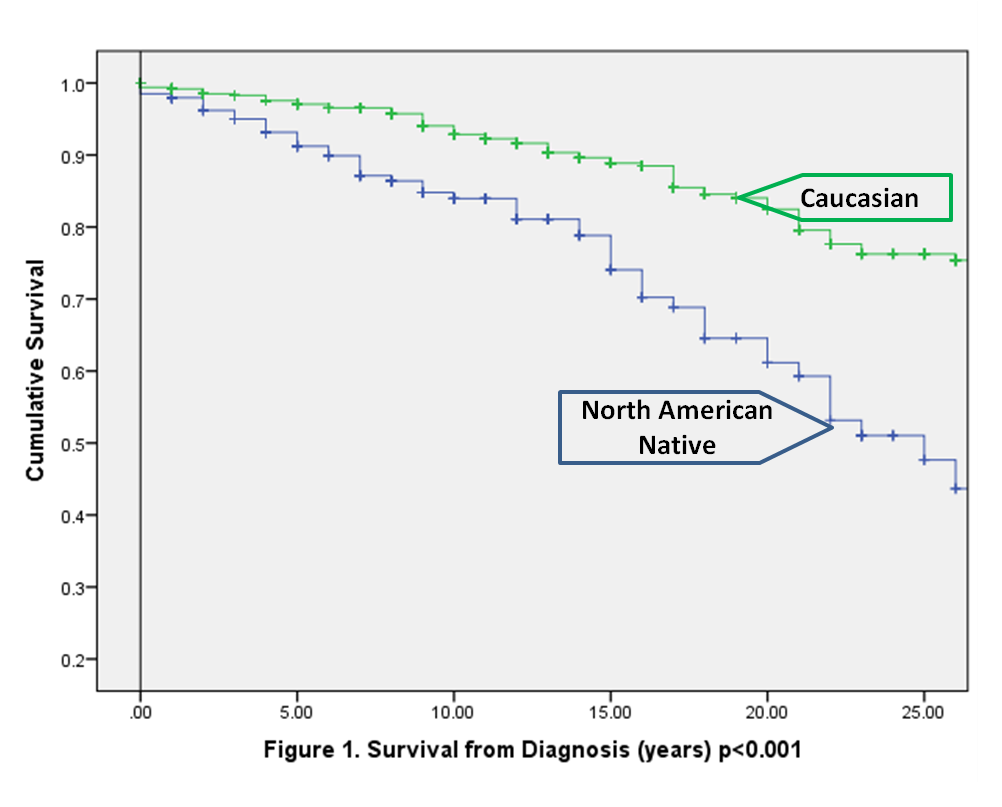
Results: A total of 861 patients with SLE were identified: 217 (25%) NAN, 534 (62%) CA, and the remaining 110 (13%) were of other ethnic backgrounds and were excluded from subsequent analyses. NAN patients were younger at diagnosis (NAN = 32±15 years vs. CA = 37±15 years; p=0.001), and had a shorter disease duration at last follow-up compared to CA (NAN = 11±8 years vs. CA = 16±10 years; p=0.001), but more NAN compared to CA were deceased by the end of the follow-up period (25% vs. 17%, p = 0.013.) Proportion of females, damage scores (SDI) and mean number of ACR criteria met (ACRc) did not differ, but NAN had more frequent nephritis (48% vs. 29%, p < 0.001) and arthritis (90% vs. 67%, p < 0.001). Mean age at death was younger in NAN (NAN = 50±16 years vs. CA = 63±16 yrs p=0.001). Survival rates were significantly worse in NAN compared to CA: 5 year survival was 92% vs. 97%; 10 year survival 85% vs. 92%; 15 year survival 78% vs. 88% respectively (p<0.001) (Figure 1).
After adjustment for ACRc, SDI, gender, age at diagnosis, disease duration, and onset decade (to account for survival bias and changes in treatment over time) NAN were more than twice as likely to die (hazard ratio 2.4; 95%CI: 1.6-3.6 ) compared to CA. PYLL for NAN (123/1000) was strikingly high compared to CA (39/1000). CA were more likely to die of atherosclerosis or malignancy (54% vs 18%), while NAN were more likely to die of lupus or lupus complications (27% vs. 16%); p= 0.005.
Conclusion: While survival in our CA patients was comparable to recent standards, we have found a twofold higher risk of mortality and threefold increase in PYLL in NAN SLE compared to CA SLE patients. Reasons for this remain unclear and highlight an urgent need for improved care delivery for NAN with SLE to decrease the significant morbidity and mortality burden from this disease.
Disclosure:
R. Puar,
None;
C. A. Hitchon,
None;
D. B. Robinson,
None;
H. El-Gabalawy,
None;
N. Dhindsa,
None;
C. A. Peschken,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/not-keeping-up-with-the-times-high-mortality-and-early-death-due-to-disease-in-north-american-natives-with-systemic-lupus-erythematosus-sle/