Background/Purpose: The proportion of patients who experience new manifestations of vasculitis after diagnosis is unknown. Our objectives were to quantify the occurrence of new features of vasculitis after diagnosis in 6 types of vasculitis and to compare patterns of disease activity over time.
Methods: Standardized data collection on 98 disease manifestations in 6 vasculitides, including granulomatosis with polyangiitis (Wegener’s, GPA), microscopic polyangiitis (MPA), Churg-Strauss syndrome (CSS), polyarteritis nodosa (PAN), giant cell arteritis (GCA), and Takayasu’s arteritis (TAK), was performed within a set of multicenter, longitudinal cohorts. For each form of vasculitis, the frequency of disease-specific manifestations at diagnosis was compared to the cumulative frequency of each manifestation. The percentage of patients who developed new “severe” manifestations after diagnosis, defined as organ-threatening or life-threatening in the small and medium vessel vasculitides and as ischemic/vascular in the large vessel vasculitides, was described.
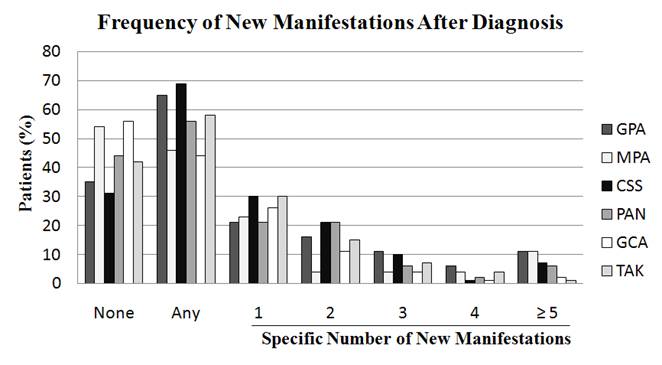
Results: The number of patients and median length of follow-up (years) for the vasculitides was: GPA 341, 7.2; MPA 26, 3.7; CSS 117, 5.1; PAN 55, 4.3; GCA 191, 2.8; TAK 132, 6.8. On average, patients with vasculitis experienced 1.3 new disease manifestations after diagnosis (GPA – 1.9, MPA – 1.2, CSS – 1.5, PAN – 1.2, GCA – 0.7, TAK – 1.0). Depending on the type of vasculitis, at least 1 new disease manifestation occurred after diagnosis in 44%-69% of patients (Figure), most notably in GPA and CSS. A subset of patients (7-28%) with each type of vasculitis experienced ≥ 3 new manifestations after diagnosis. The 3 most frequent new manifestations after diagnosis for each type of vasculitis are listed in the Table. New severe manifestations occurred after diagnosis in GPA – 30%, MPA – 27%, CSS – 23%, PAN – 29%, GCA – 26%, and TAK – 45%. Mean time from diagnosis to initial flare in disease activity did not significantly differ among those who experienced a new manifestation versus a recurrence of prior disease (1.15 vs 1.18 years, p=0.8).
Conclusion: A majority of patients with vasculitis develop new features of disease after diagnosis, including a substantial number of new, severe manifestations. New manifestations after diagnosis, although more frequent among the small-vessel vasculitides, are also common in patients with medium- or large-vessel vasculitis. Patterns of disease recurrence after diagnosis are not related to disease duration. Ongoing clinical assessment of patients with all types of established vasculitis should remain broad in scope.
|
Three Most Frequent New Manifestations After Diagnosis |
|
|
Type of Vasculitis |
New Manifestation |
|
Granulomatosis with polyangiitis |
Arthralgias (11%) Rhinitis (9%) Glomerular disease (9%) |
|
Microscopic polyangiitis |
Venous thromboembolic event (12%) Glomerular disease (11%) Arthalgias (8%) |
|
Churg-Strauss syndrome |
Nasal polyp (10%) Eosinophilic pulmonary infiltrate (9%) Purpura (8%) |
|
Polyarteritis nodosa |
Motor mononeuritis multiplex (12%) Arthralgias (12%) Venous thromboembolic event (10%) |
|
Giant cell arteritis |
Polymyalgia rheumatica (11%) Headache (7%) Arthralgias (7%) |
|
Takayasu’s arteritis |
Upper extremity claudication (14%) Lightheadedness (8%) Carotidynia (7%) |
Disclosure:
P. C. Grayson,
None;
D. Cuthbertson,
None;
S. Carette,
None;
G. S. Hoffman,
None;
N. A. Khalidi,
None;
C. L. Koening,
None;
C. A. Langford,
None;
K. Maksimowicz-McKinnon,
None;
P. A. Monach,
None;
P. Seo,
None;
U. Specks,
None;
S. R. Ytterberg,
None;
P. A. Merkel,
None.
« Back to 2012 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/new-disease-manifestations-after-diagnosis-in-six-types-of-vasculitis/