Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: The new 2019 SLE EULAR/ACR Classification Criteria for Systemic lupus erythematosus (SLE) have been developed to find a better equilibrium between specificity and sensitivity compared to SLE ACR-1997 and SLE SLICC. Given the biological and clinical similarities and the frequent overlap between SLE and primary Sjögren’s Syndrome (pSS), these criteria could be useful in clinical practice for differentiating SLE from pSS.
The aim of this study was to explore the utility of the 2019 SLE EULAR/ACR criteria compared to SLE ACR-1997 and SLE SLICC criteria for differentiating in clinical practice SLE from pSS and overlap between both.
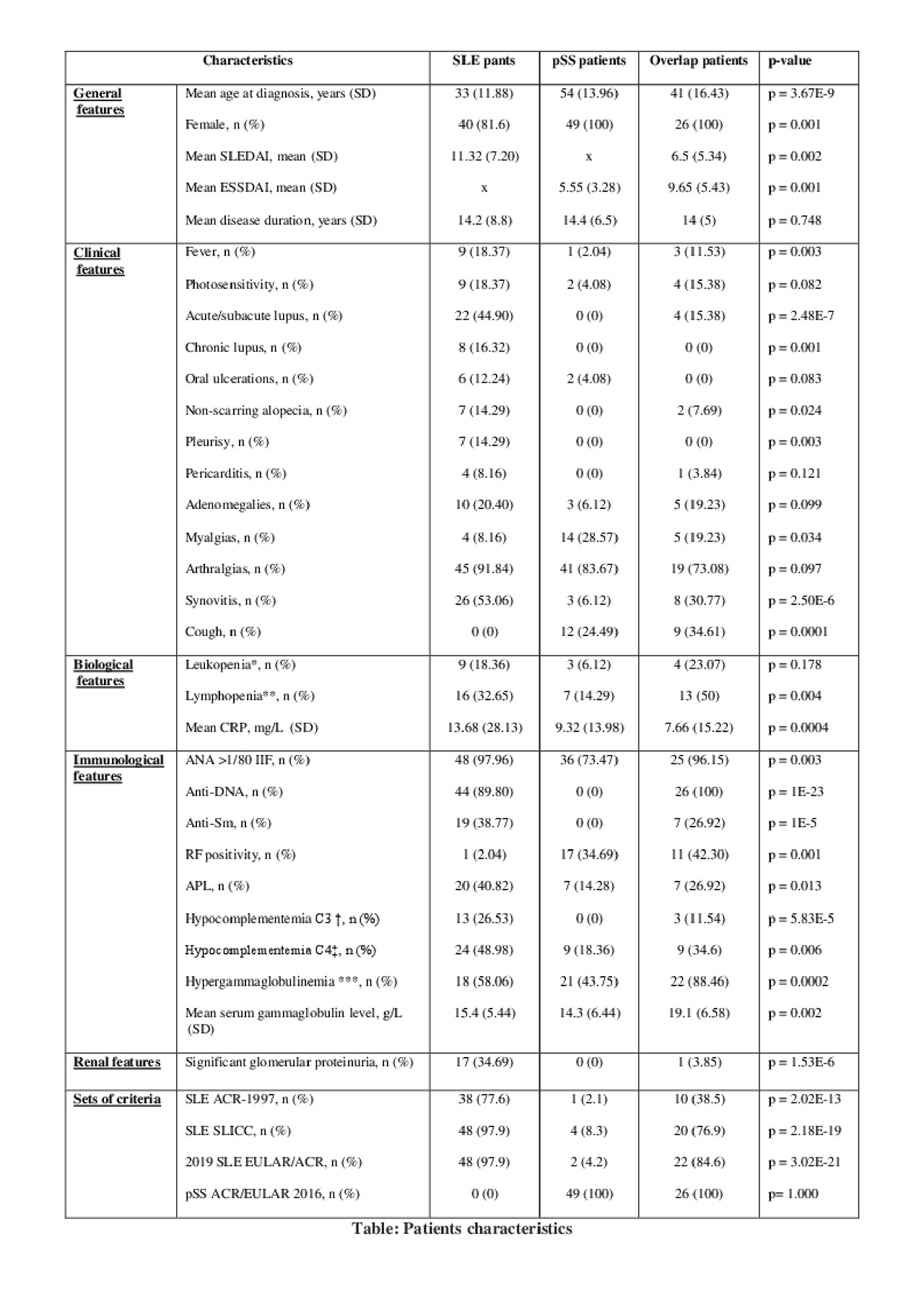
Methods: This retrospective study included 3 different groups of patients followed in Department of Rheumatology, Hopitaux Universitaires Paris Sud: (i) 49 SLE patients (diagnosis made by the clinician with exclusion of patients with another connective tissue disease associated). (ii) 49 pSS patients randomly chosen from the Paris Sud database, fulfilling the pSS ACR/EULAR 2016 criteria, with exclusion of patients with association of another connective tissue disease (iii) 26 SLE/Sjögren’s Syndrome (SS) overlap patients based on clinical diagnosis, made of 13 patients diagnosed as SLE and presenting objective signs of associated SS (minor salivary glands biopsy Focus Score ≥ 1, and/or objective sicca syndrome) and 13 patients diagnosed as SS with anti-DNA antibodies.
The biological, immunological, and clinical data were collected at diagnosis, or at the first visit at the centre. SLE ACR-1997, SLE SLICC and 2019 SLE EULAR/ACR criteria were tested in each group. Categorical variables were compared using a Chi² or Fischer’s exact test as appropriate. Quantitative variables were compared with Kruskal-Wallis test.
Results: As shown in Table, the 2019 SLE EULAR/ACR criteria were met in 97.9% of the SLE patients vs 4.2% of the pSS patients (p< 0.001). Interestingly, patients from the overlap group fulfilled both criteria for SLE and SS confirming the capacity of the criteria to detect the overlap. Lymphopenia and biological inflammation were significantly associated with SLE (respectively 33% vs 14%, p=0.004 and 28% vs 14%, p< 0.001), whereas initial rheumatoid factor detection was significantly associated with pSS (3.5% vs 35%, p=0.001). Systematic assessment of sicca syndrome could help to differentiate SLE from pSS. Overlap syndrome patients had a more systemic disease than pSS patients as assessed by the EULAR Sjögren’s syndrome Disease Activity Index (ESSDAI): respectively 5.6 vs 9.7 (p=0.001).
Conclusion: In conclusion this study shows that the new 2019 SLE EULAR/ACR criteria for SLE can be useful in clinical practice helping to differentiate between SLE and pSS and detecting overlap presentations.
CRP: C-reactive protein, ANA: antinuclear antibodies, ESSDAI4: EULAR Sjögren’s syndrome Disease Activity Index, SLEDAI5: Systemic Lupus Erythematosus Disease Activity Index, ACR: American College of Rheumatology, SLICC: Systemic Lupus International Collaborating Clinics, EULAR: European League Against Rheumatism,
*Leukopenia was defined by leukocytes count < 4000/mm3
**Lymphopenia was defined by lymphocytes count < 1000/mm3
***Hypergammaglobulinemia was defined by serum gammaglobulin level > 13.5 g/L
C3† and C4‡ hypocomplementemia were defined by seric C3 and C4 fractions levels ≤ 0.5 g/L and 0.15 g/L, respectively.
Significant glomerular proteinuria was defined by daily proteinuria ≥ 1g /day
To cite this abstract in AMA style:
Assan F, Seror R, Nocturne G, Mariette X. New 2019 SLE EULAR/ACR Classification Criteria for SLE Are Valuable for Distinguishing Patients with SLE from Patients with pSS in Daily Practice [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/new-2019-sle-eular-acr-classification-criteria-for-sle-are-valuable-for-distinguishing-patients-with-sle-from-patients-with-pss-in-daily-practice/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/new-2019-sle-eular-acr-classification-criteria-for-sle-are-valuable-for-distinguishing-patients-with-sle-from-patients-with-pss-in-daily-practice/