Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Temporal artery biopsy (TAB) plays a key role in diagnosis of giant cell arteritis (GCA). However, approximately 15-20% of patients ultimately diagnosed with GCA have negative biopsies. Among patients with negative TAB, it is often challenging to identify patients with GCA from those with an alternate (non-GCA) diagnosis. Therefore, we sought to compare TAB-negative GCA with patients receiving a non-GCA alternate diagnosis.
Methods: Two cohorts were retrospectively identified through direct medical record review. The first cohort consisted of patients with TAB-negative GCA diagnosed between 1/1/1998 and 12/31/2013. The second cohort included all patients with a negative TAB performed between 1/1/2009 and 12/31/2010 in which a non-GCA alternate diagnosis was provided after a minimum of 6 months of follow up. Final diagnoses were confirmed by consensus among two rheumatologists and a physician abstractor. Baseline characteristics were compared between the two cohorts using chi-square and rank sum tests.
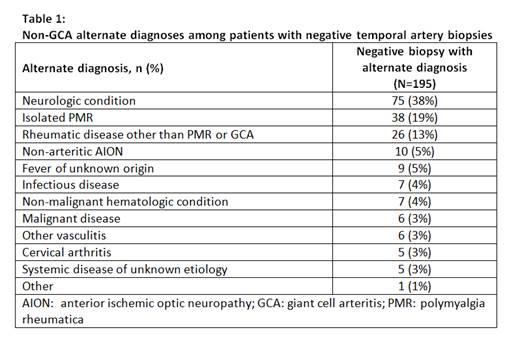
Results: 110 patients with TAB-negative GCA and 195 non-GCA patients with a negative TAB were identified. Alternate diagnoses for non-GCA patients are listed in Table 1. Age, sex, number of days on glucocorticoids prior to biopsy, and biopsy length were similar in both groups. Time from first symptom to diagnosis was longer in non-GCA patients [mean (SD); 2.6 (2.5) vs 1.5 (2.1) months; p<0.001] and fewer non-GCA patients fulfilled ≥3 ACR criteria for GCA (27% vs 64%; p<0.001). Although headache was the primary symptom in both cohorts (66% TAB-negative GCA; 68% non-GCA), patients with biopsy-negative GCA had more frequent anorexia, fatigue, fever, polymyalgia rheumatica, temporal artery tenderness and claudication (jaw, arm, or leg). Baseline transient (5% TAB-negative GCA; 6% non-GCA; p=0.58) and permanent (3% TAB-negative GCA; 3% non-GCA; p=0.86) vision loss were infrequently observed. ESR was higher in TAB-negative GCA patients [64.0 (35.1) vs 55.2 (67.4) mm/hr; p=0.002] compared to non-GCA patients but CRP did not differ [44.3 (53.6) vs 43.8 (61.9) mg/L; p=0.39].
Conclusion: In this cohort, neither headache nor vision loss at presentation were associated with an ability to discriminate between diagnosis of TAB-negative GCA compared to patients without GCA. ACR criteria may be helpful in identifying patients with TAB-negative GCA. Among patients with negative TAB, constitutional symptoms and claudication (jaw/limb) were more frequently associated with an ultimate diagnosis of TAB-negative GCA.
To cite this abstract in AMA style:
Yeruva K, Warrington KJ, Crowson CS, Koster MJ. Negative Temporal Artery Biopsies: Comparison between Biopsy-Negative GCA and Non-GCA Patients [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/negative-temporal-artery-biopsies-comparison-between-biopsy-negative-gca-and-non-gca-patients/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/negative-temporal-artery-biopsies-comparison-between-biopsy-negative-gca-and-non-gca-patients/