Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Septic arthritis is a rheumatologic emergency associated with significant morbidity and mortality. This study examines the descriptive characteristics and risk factors associated with in-hospital mortality among those with non-gonococcal bacterial knee septic arthritis using a large U.S. claims-based inpatient database.
Methods: A retrospective study of all adult hospitalizations with non-gonococcal bacterial knee septic arthritis from National Inpatient Sample (NIS) between 2016 and 2020 was conducted. Cases were identified by ICD-10 codes M00.06, M00.16, M00.26 and M00.86. Prosthetic joint infections and gonococcal septic arthritis were excluded. A univariable screen was done for potential risk factors for in-hospital death. All variables with p ≤ 0.2 were included in a multivariable logistic regression model and were considered significant at a p ≤ 0.05. Charlson Comorbidity Index (CCI) was used to adjust for comorbidity burden.
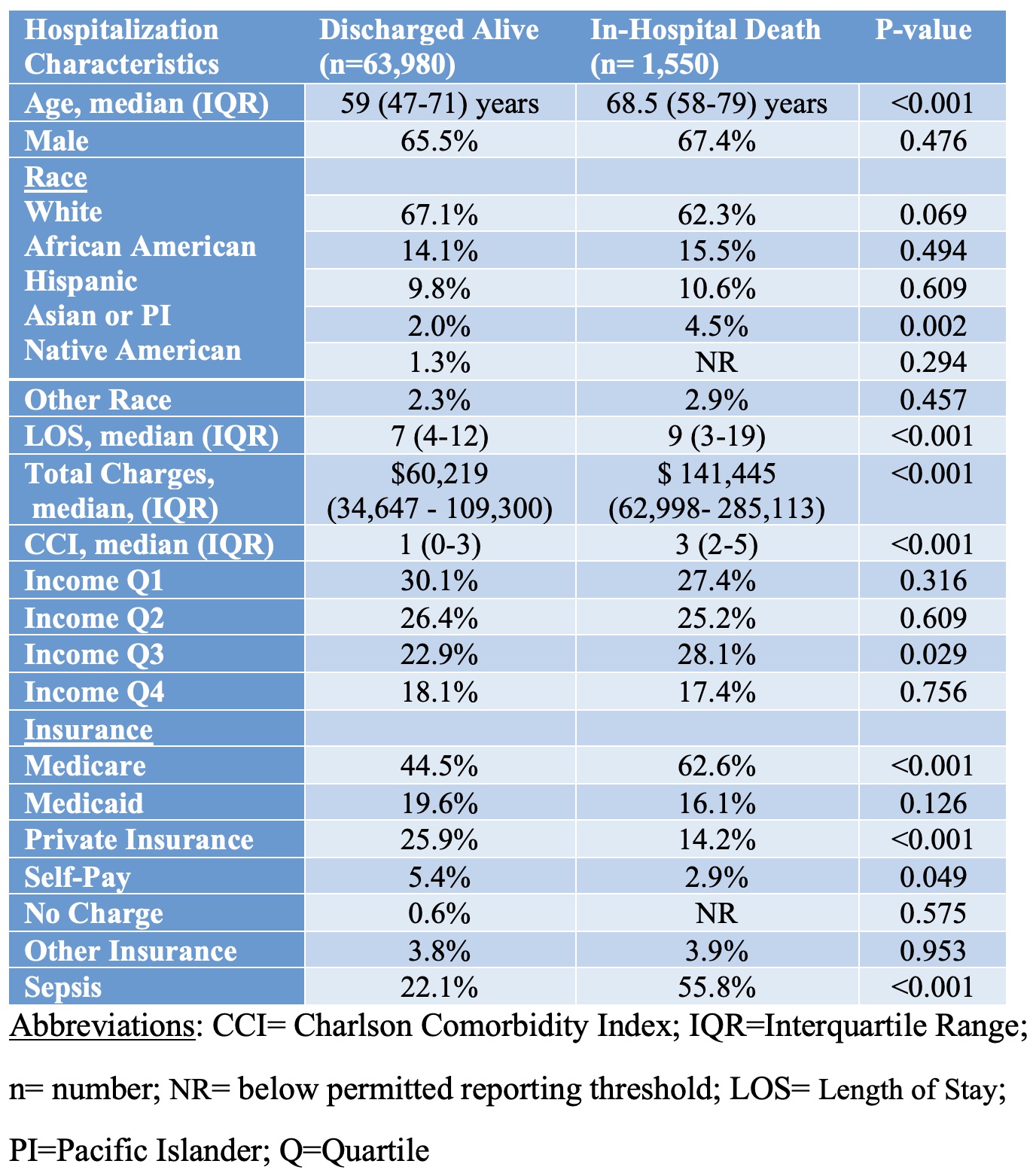
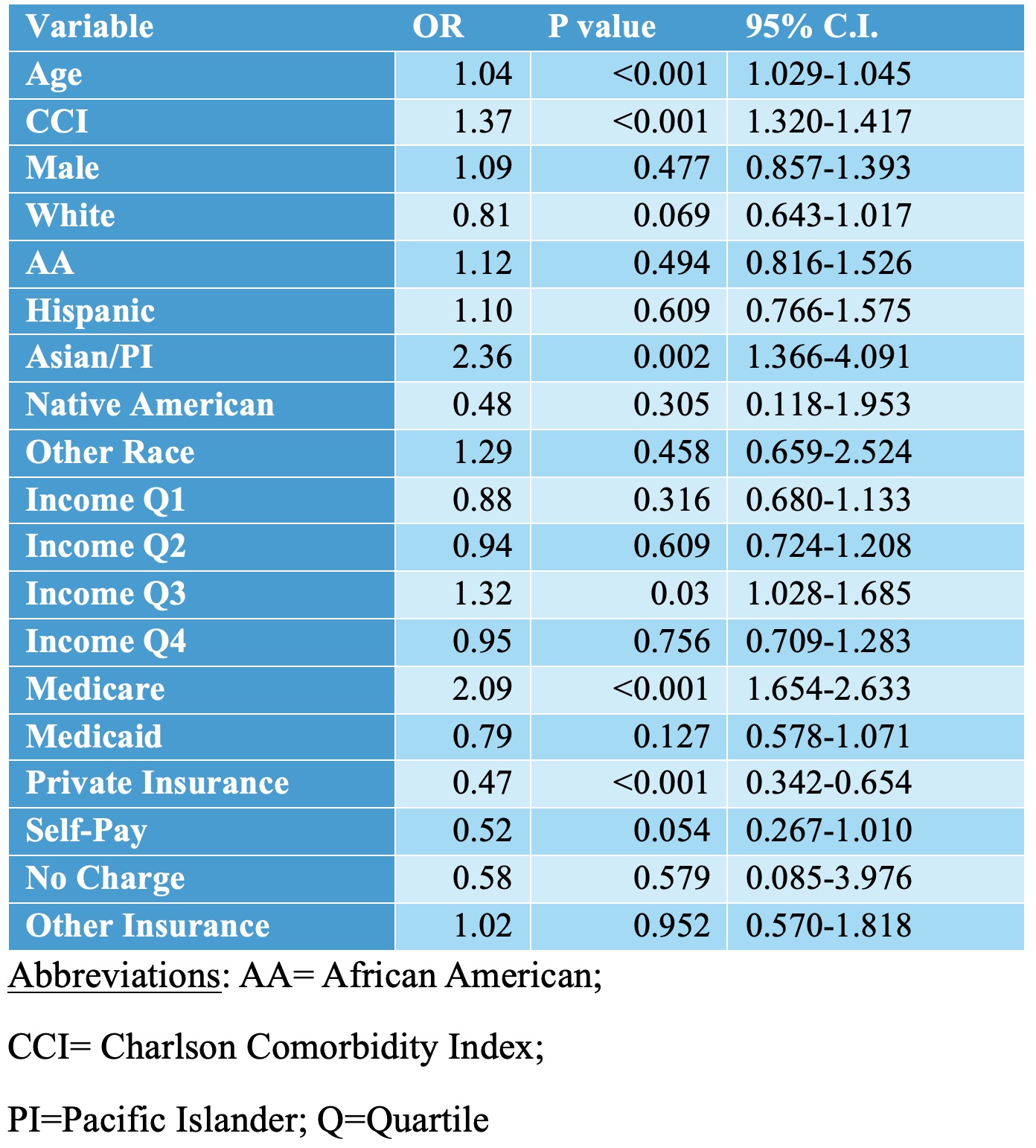
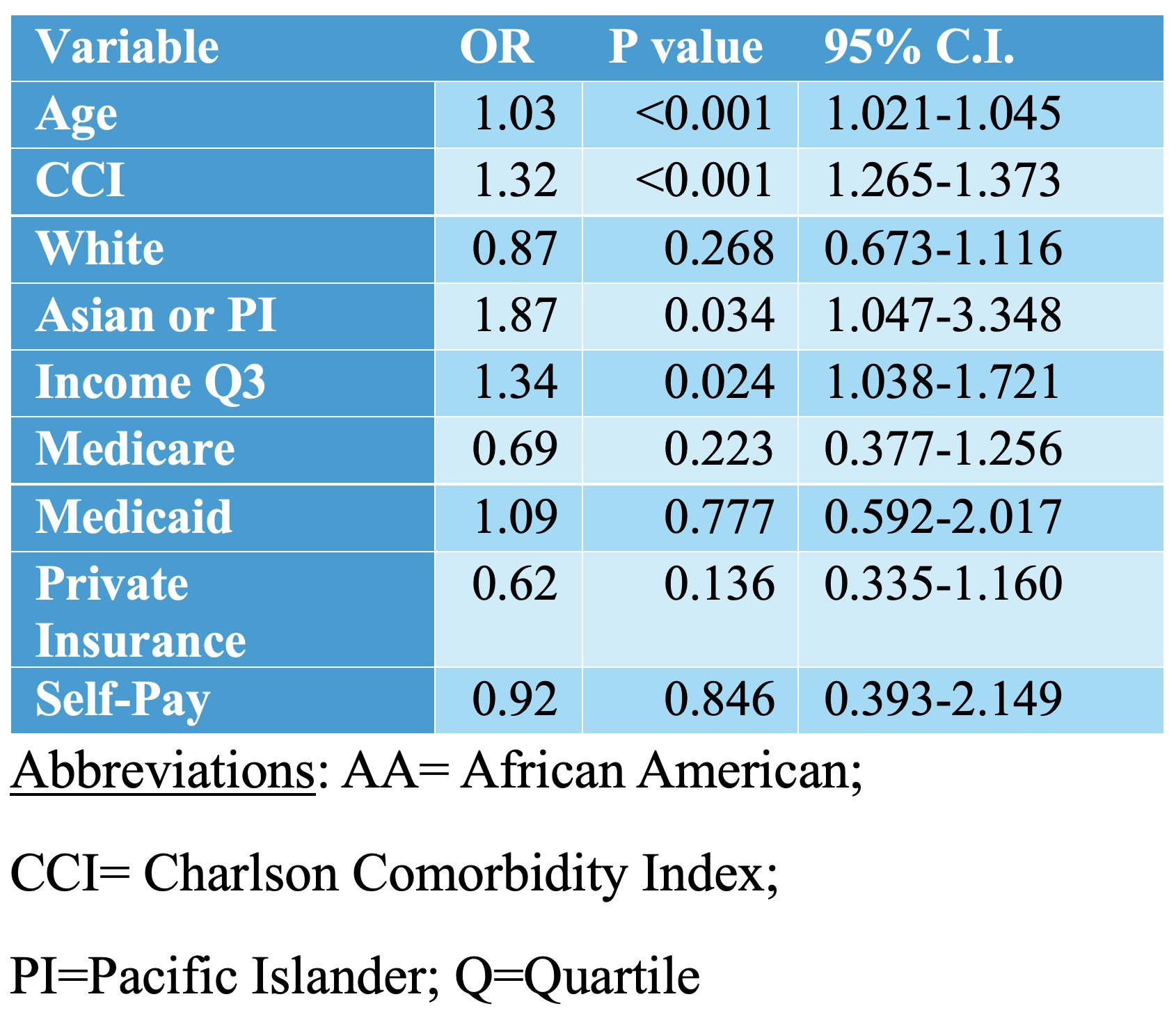
Results: There were 65,595 septic arthritis knee hospitalizations from 2016 to 2020 (table 1). Of those, 63,980 (97.6%) were discharged alive and 1,550 (2.4%) died in the hospital. Mortality data was not available for 65 patients. Patients who died the in-hospital were older (median age 68.5 vs. 59 years, p< 0.001), had longer median hospital length of stays (LOS) (9 vs. 7 days, p< 0.001), higher total median hospital charges ($141,445 vs. $60,219, p< 0.001), greater median CCI (3 vs. 1, p< 0.001), more Asian/Pacific Islanders (PI) (4.5% vs. 2.0%, p=0.002), more Medicare (62.6% vs. 44.5%, p< 0.001), less private insurance (14.2% vs. 25.9%, p< 0.001), and more concurrent sepsis (55.8% vs. 22.1%, p< 0.001). Multivariable analysis identified several significant predictors of in-hospital death among those with septic knee arthritis including increasing age (OR 1.03; 95% CI 1.021-1.045), higher CCI (OR 1.32; 95% CI 1.265-1.373), Asian/PI (OR 1.87; 95% CI 1.047-3.348) and household income quartile 3 (OR 1.34; 95% CI 1.038-1.721) (Tables 2 and 3).
Conclusion: In-hospital mortality for non-gonococcal native knee bacterial septic arthritis was 2.4%. Those that died in the hospital had longer LOS, greater hospital charges, and more concurrent sepsis. Variables independently associated with higher odds of in-hospital death were older age, greater comorbidity burden, Asian/PI ethnicity, and income quartile 3. These findings highlight the need for targeted interventions to improve mortality in high-risk septic arthritis populations.
To cite this abstract in AMA style:
Tanveer S, Manadan A, Cornejo-Gonzalez D. Nationwide Analysis of Adult Non-Gonococcal Bacterial Septic Arthritis Hospitalizations from the National Inpatient Sample 2016 to 2020 [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/nationwide-analysis-of-adult-non-gonococcal-bacterial-septic-arthritis-hospitalizations-from-the-national-inpatient-sample-2016-to-2020/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/nationwide-analysis-of-adult-non-gonococcal-bacterial-septic-arthritis-hospitalizations-from-the-national-inpatient-sample-2016-to-2020/