Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Infection is a major cause of morbidity and mortality in systemic lupus erythematosus (SLE). With changing therapeutic practices over the past 15 years, it is unknown whether infectious complications of SLE have also evolved. In this study, we used the Healthcare Cost and Utilization Project National Inpatient Sample (NIS) to evaluate trends in hospitalizations for severe infections in SLE patients.
Methods: Using data from the 2000 to 2011 NIS, a nationally representative 20% sample of all US hospitalizations, we compared hospitalizations among individuals ≥ age 18 who met a validated administrative definition of SLE to hospitalizations of non-SLE patients. Primary outcomes were a discharge diagnosis of a severe infection (bacteremia, pneumonia, opportunistic fungal infection, herpes zoster (VZV), cytomegalovirus, or pneumocystis jirovecii pneumonia (PCP)). Direct standardization was used to generate annual rates of infection in SLE hospitalizations adjusted for age, gender, and a modified Charlson Comorbidity Index in comparison to non-SLE hospitalizations. Adjusted logistic regression models with an effect modification term for SLE and year were used to investigate differences in rates of infections over time among SLE vs. non-SLE hospital discharges.
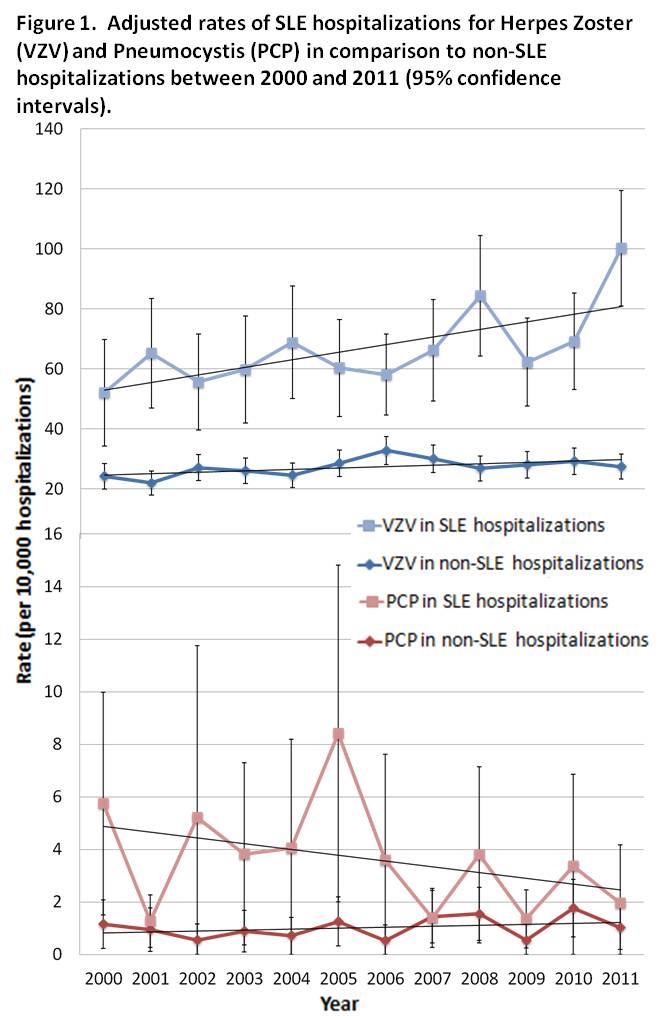
Results: We identified 361,484 hospitalizations for SLE between 2000 and 2011. Compared to non-SLE hospitalized patients, SLE patients were younger (51 vs. 62 years) and predominantly female (89% vs. 54%), but had a similar comorbidity index (1.2 for both groups). In adjusted logistic regression analyses, a diagnosis of SLE was significantly associated with discharge diagnoses for bacteremia (OR 1.5, 95% CI 1.5-1.6), pneumonia (OR 1.3, 95% CI 1.2-1.3), fungal infections (OR 3.0, 95% CI 2.8-3.2), VZV (OR 2.0, 95% CI 1.9-2.2), cytomegalovirus (OR 5.0, 95% CI 4.2-6.1), and PCP (OR 3.7, 95% CI 2.7-5.1). Between 2000 and 2011, hospitalizations for VZV in patients with SLE increased more rapidly than rates in the non-SLE population, from 52 to 100 cases per 10,000 SLE admissions compared to 24 to 27 cases per 10,000 non-SLE admissions, even after adjustment (p for effect modification 0.036, Figure 1). Conversely, hospitalizations for PCP in SLE decreased over time, from an adjusted rate of 5 to 2 per 10,000 admissions, but remained stable at 1 per 10,000 in the non-SLE population (p for effect modification 0.021).
Conclusion: Among patients with SLE, hospitalizations for VZV are rising at a rate disproportionate to the non-SLE population, while hospitalizations for PCP in SLE are declining. These trends likely reflect changing immunosuppressive treatments and practice patterns in SLE, although further research is needed to determine which therapies significantly affect risk.
Disclosure:
S. G. Murray,
None;
G. Schmajuk,
None;
L. Trupin,
None;
L. S. Gensler,
UCB,
5,
AbbVie,
5,
Celgene Corporation,
9;
J. Yazdany,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/national-hospitalization-trends-in-lupus-reveal-rising-rates-of-herpes-zoster-and-declines-in-pneumocystis-infections/