Session Information
Date: Wednesday, November 8, 2017
Title: Vasculitis III: Pathogenesis
Session Type: ACR Concurrent Abstract Session
Session Time: 9:00AM-10:30AM
Background/Purpose:
Prior studies have suggested a potential link between nasal microbes, in particular Staphylococcus aureus, and granulomatosis with polyangiitis (GPA; Wegener’s) but these studies relied on culture-dependent methods. This study comprehensively examined the entire community of nasal microbiota in patients with GPA compared to healthy controls using deep sequencing methods.
Methods:
The nasal microbiota of 61 patients with GPA and 41 healthy controls was sampled using nasal swabs and analyzed by sequencing of the bacterial 16S rRNA gene (V1-V2 region). The abundance profiles of the 11 most abundant bacterial taxa were compared using the Wilcoxon rank sum test, correcting for multiple comparisons. Additional comparative analyses within the GPA cohort were performed by ANCA type (PR3 vs MPO), presence or absence of sinonasal Vasculitis Damage Index items (VDI), and disease activity (active vs remission). The effects of antibiotics and immunosuppressive therapies (both current and within the past 6 months) were evaluated using generalized linear models.
Results:
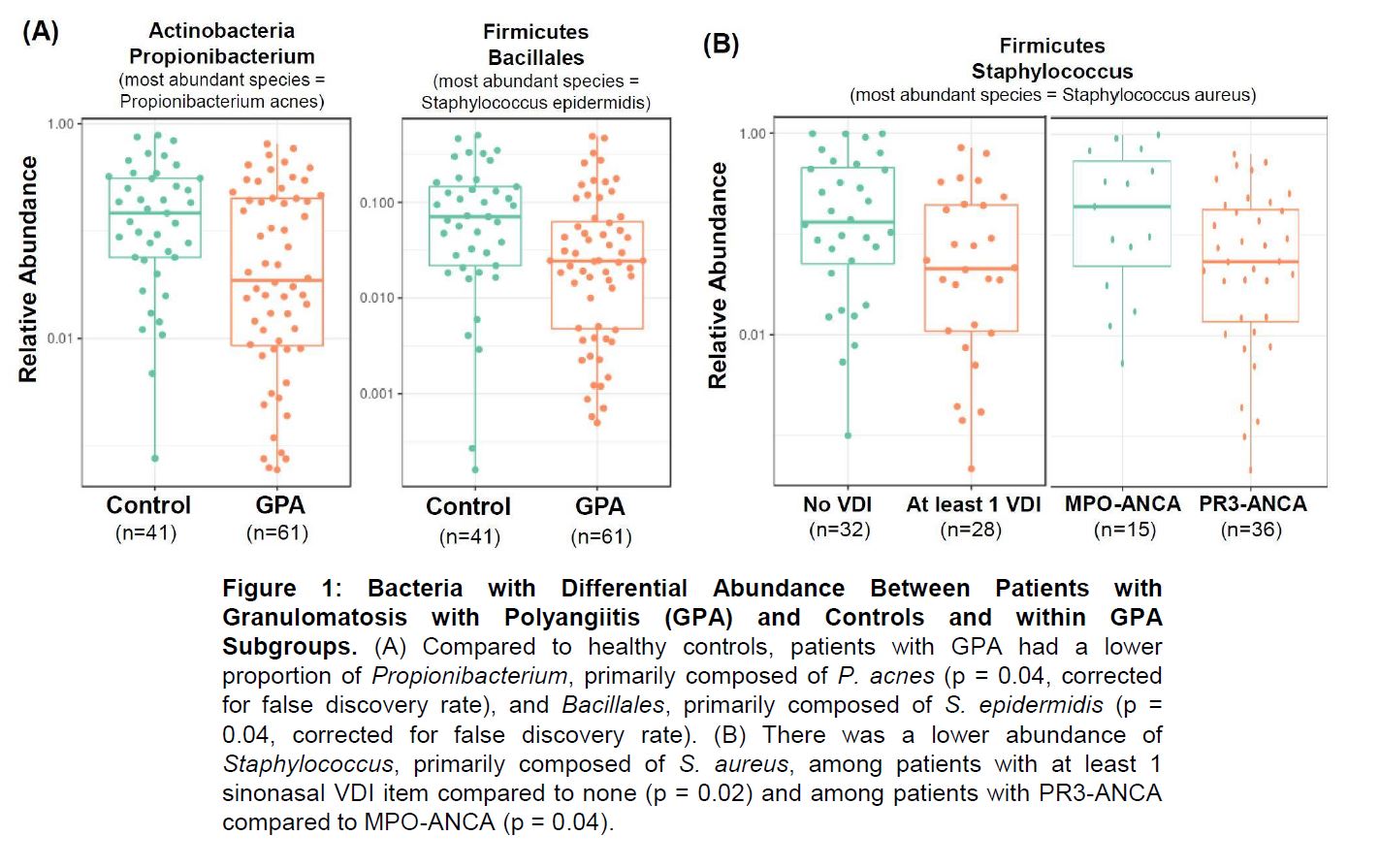
Corynebacterium, Propionibacterium, and Staphylococcus featured as prominent bacterial taxa in the nasal swab samples, consistent with previous reports. After clustering the sequence reads into operational taxonomic units, we identified two abundant groups of Staphylococcus in the data: one closely related to S. aureus and the other similar to S. epidermis. The S. epidermis cluster and Propionibacterium were decreased in abundance in GPA vs controls (Figure 1A). In multivariate analyses, patients with GPA receiving non-glucocorticoid immunosuppressive therapy had a higher abundance of Propionibacterium (p = 0.01) that was similar to the abundance seen in healthy controls. Among patients with GPA, there was a lower abundance of the S. aureus cluster in i) subjects with PR3- vs MPO-ANCA; and ii) subjects with at least 1 sinonasal VDI item vs. those without a sinonasal VDI item (Figure 1B). In multivariate analyses, ANCA type remained significantly associated with abundance of S. aureus independent of medications and presence of a sinonasal VDI item (p = 0.01).
Conclusion:
Nasal microbial communities differ between patients with GPA and controls as well as between clinically-distinct subsets of GPA. Interestingly, a lower abundance of Propionibacterium (which prior studies have suggested may negatively interact with S. aureus) was found in patients with GPA, particularly among those off immunosuppressive therapies, raising the possibility that a loss of the “protective” effect of Propionibacterium may increase susceptibility to colonization by pathogens such as S. aureus. These data support the theory that microbes are involved in the disease process of GPA and that a deeper understanding of dysbiotic microbial communities in GPA could lead to novel preventative or therapeutic strategies.
To cite this abstract in AMA style:
Rhee RL, Sreih AG, Najem CE, Grayson PC, Zhao C, Bittinger K, Collman RG, Merkel PA. Nasal Microbiota in Patients with Granulomatosis with Polyangiitis Compared to Healthy Controls [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/nasal-microbiota-in-patients-with-granulomatosis-with-polyangiitis-compared-to-healthy-controls/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/nasal-microbiota-in-patients-with-granulomatosis-with-polyangiitis-compared-to-healthy-controls/