Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Nailfold videocapillaroscopy (NVC) is a non-invasive tool used to evaluate the microcirculation of patients with connective tissue diseases (CTDs). A specific combination of NVC abnormalities, known as the “scleroderma pattern,” has been well-described in patients with systemic sclerosis and demonstrated to have prognostic significance. The significance of these changes in patients with idiopathic inflammatory myopathies (IIMs) has yielded conflicting results. The primary objective of this analysis was to assess the significance of NVC abnormalities in a North American, single-center cohort of IIM patients.
Methods: Sixty-seven adult patients with IIM, 65 of whom met 2017 EULAR/ACR classification criteria for IIM, were enrolled for participation between October 2020 and October 2021. Clinical and demographic characteristics and validated core set measures, including the Myositis Disease Activity Assessment Tool (MDAAT), Myositis Damage Index (MDI), and Manual Muscle Testing (MMT8), were obtained for each patient. NVC was performed on eight fingers per patient (two images per finger) by a single examiner using a digital optical probe videocapillaroscope at 200x magnification and analyzed using a standardized method derived by consensus from the EULAR Study Group on Microcirculation in Rheumatic Diseases. Quantitative and qualitative assessments of NVC images were made by two trained examiners using the “Fast Track Algorithm” developed by the EULAR Study Group. Descriptive statistics were performed, and comparisons were calculated using Fisher’s exact test, T-tests, Wilcoxon rank sum tests, and ANOVA as appropriate. An alpha level of 0.05 was used to determine statistical significance.
Results: Of the 67 patients, 35 (52%) had dermatomyositis (DM), 24 (36%) had polymyositis (PM) and 8 (12%) had inclusion-body myositis (IBM). Fifteen (22%) of the patients had defined scleroderma patterns on NVC; 11 of these 15 patients had DM. The remaining patients had non-scleroderma patterns on NVC, and all demonstrated at least one non-specific abnormality.
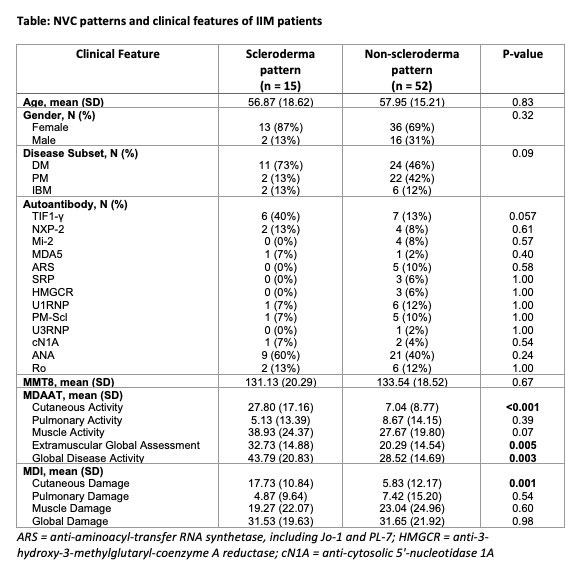
Patients with scleroderma patterns on NVC had significantly higher MDAAT cutaneous activity compared to those with non-scleroderma patterns (p < 0.001). Patients with scleroderma patterns also had more active disease overall, as measured by the MDAAT global disease activity (p=0.003). Additionally, those with scleroderma patterns had significantly higher MDI cutaneous damage (p = 0.001). Anti-TIF1-γ positivity was more frequently observed in those with scleroderma patterns than in those without, though this did not reach statistical significance (40% vs. 13%, p = 0.057) (Table).
Conclusion: This is the first standardized evaluation of nailfold videocapillaroscopy in an IIM cohort. Scleroderma patterns on NVC were observed in 22% of these patients and were associated with higher overall disease activity, cutaneous disease activity, and cutaneous damage. Larger studies are needed to determine whether NVC abnormalities associate with other valuable clinical characteristics, particularly autoantibody profiles.
To cite this abstract in AMA style:
Zisa D, Bloostein A, Jannat-Khah, DrPH, MSPH D, Cutolo M, Smith V, Fernandez D. Nailfold Videocapillaroscopic Abnormalities Correlate with Disease Activity Measures and Cutaneous Damage in Patients with Idiopathic Inflammatory Myopathies [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/nailfold-videocapillaroscopic-abnormalities-correlate-with-disease-activity-measures-and-cutaneous-damage-in-patients-with-idiopathic-inflammatory-myopathies/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/nailfold-videocapillaroscopic-abnormalities-correlate-with-disease-activity-measures-and-cutaneous-damage-in-patients-with-idiopathic-inflammatory-myopathies/