Session Information
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Myositis-specific antibodies (MSAs) are identified in over half of children with JDM and are associated with distinct clinical phenotypes. MSA subtype, in combination with clinical or muscle histopathology findings, may have prognostic value and implications for disease monitoring and treatment. The aim of this study is to define the relationships between MSAs and muscle histopathology as well as clinical markers of disease activity in children with JDM.
Methods: A retrospective chart review of subjects with JDM followed in the pediatric rheumatology clinic at a single center between October 2016 and November 2018 was performed. Markers of JDM disease activity, including muscle enzymes (creatine kinase (CK), aldolase, lactate dehydrogenase, aspartate aminotransferase, and alanine transaminase) and other clinical data were obtained at the initial visit and at 6 months. MSA serum levels were measured at a single point during the disease course. Muscle biopsy samples, routinely obtained at diagnosis, were reviewed and scored independently by 2 neuropathologists using a visual analog scale. Mann-Whitney tests were conducted to detect differences between the most prevalent MSA subtypes. Pearson correlation coefficient (r) was conducted to analyze the correlation between MSA subtype and CK.
Results: Out of the 43 subjects in the study, 26 (60.5%) had a detectable MSA. The most common MSAs were anti-NXP-2 (13, 30.2%), anti-Mi-2 (7, 16.3%), and anti-MDA-5 (5, 11.6%). Other MSAs detected included anti-SRP, anti-Tif-1g, anti-OJ, and anti-PL-7.
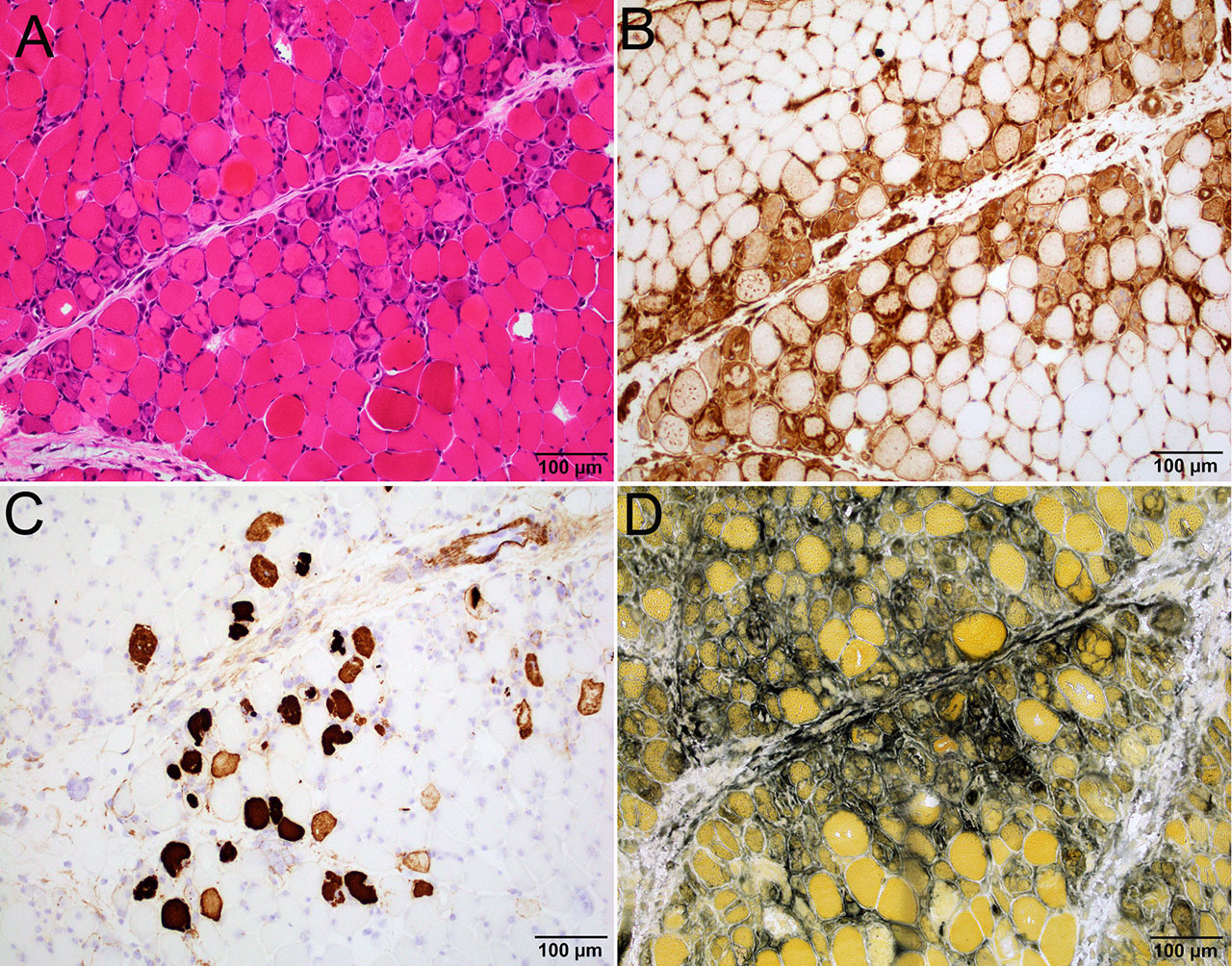
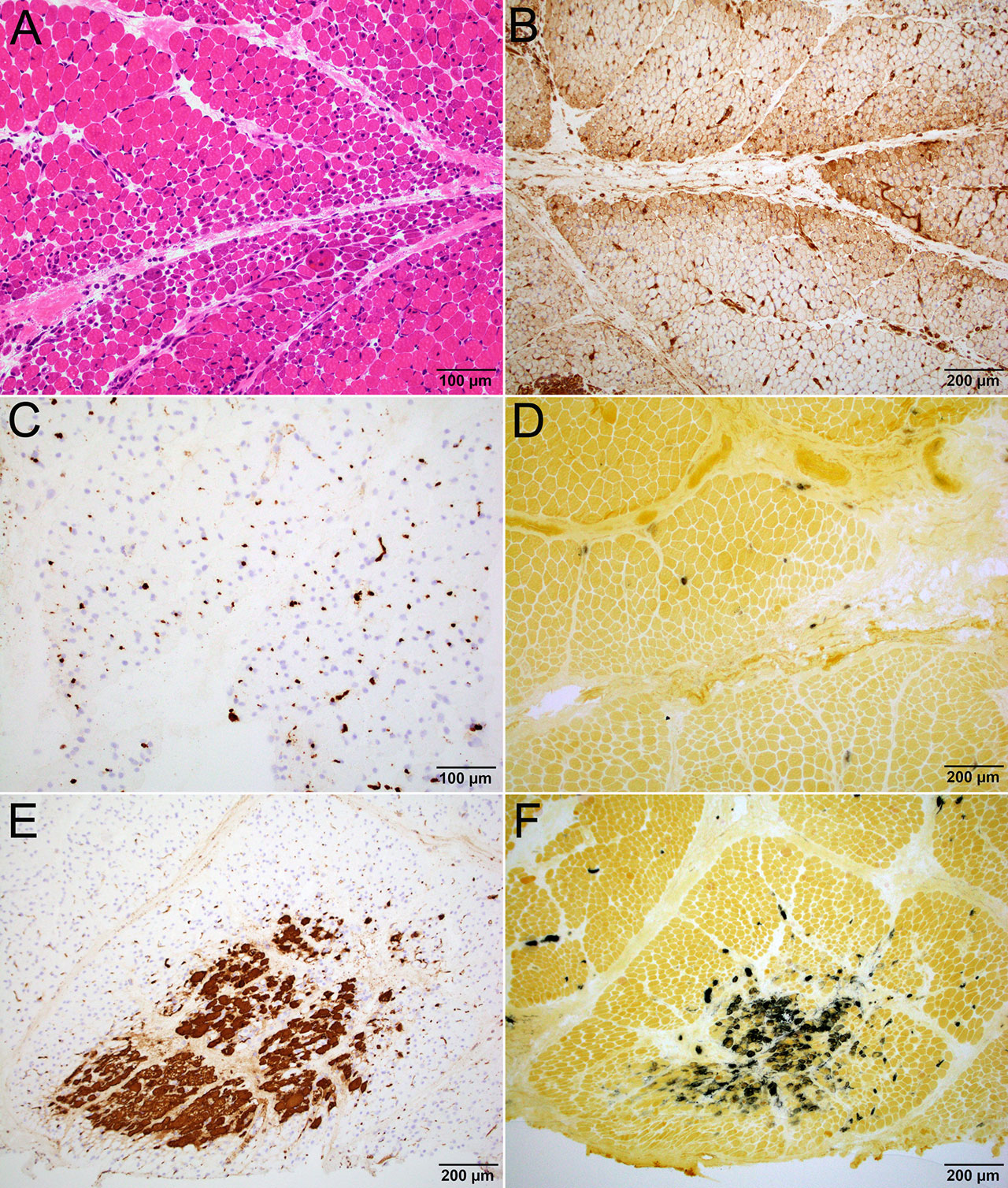
Subjects with high titer anti-Mi-2 had more widespread perifascicular myofiber damage and perifascicular necrotizing myopathy (Figure 1). Subjects with high titer anti-NXP-2 had more prominent capillary C5b-9 deposition, indicative of vascular injury, and myofibers showed perifascicular atrophy and/or focal infarct but minimal perifascicular myofiber necrosis (Figure 2). All subjects with anti-MDA-5 had normal CK and normal muscle histology, consistent with previous reports of amyopathic or hypomyopathic disease. The subject with anti-PL-7 showed perifascicular necrotizing myopathy with diffuse MHC-1 upregulation on histopathology, consistent with the pattern seen in antisynthetase syndrome.
High titer anti-Mi-2 correlates with serum CK > 10,000 (r=0.96, p=0.002) (Figure 3). With the exception of a subject with anti-PL-7, no other MSA subtypes had a CK > 5000 at the initial visit. Anti-Mi-2 had a higher CK at initial visit compared to anti-NXP-2 (p=0.04) and anti-MDA-5 (p=0.05). In general, anti-Mi-2 was significantly associated with higher muscle enzymes, except for aldolase. There is no correlation between anti-NXP-2 titer and CK (r=-0.21, p=0.49) (Figure 3).
Conclusion: The mechanism of injury for patients with JDM differs based on MSA subtype: anti-Mi-2 is associated with direct myofiber damage; anti-NXP-2 is associated with vascular injury; and anti-MDA-5 is associated with minimal to no muscle injury. Serum CK, a clinical marker of disease activity, varies based on MSA subtype: anti-Mi-2 titer correlates with serum CK; anti-NXP-2 titer does not correlate with serum CK; and anti-MDA-5 is associated with normal serum CK.
-A- H&E shows abundant necrotic and regenerating fibers concentrated in perifascicular region.
-B- MHC-1 is upregulated in perifascicular myofibers.
-C- C5b-9 highlights necrotic fibers. There is no significant capillary deposition.
-D- Alkaline phosphatase shows strong reactivity in regenerating fibers as well as in perimysial and endomysial connective tissue.
-A- H&E shows prominent perifascicular atrophy without significant myofiber necrosis.
-B- MHC-1 is upregulated in perifascicular myofibers.
-C- C5b-9 shows prominent capillary C5b-9 deposition.
-D- Alkaline phosphatase shows no regenerating fibers or connective tissue reactivity.
-E-F- Focal area of infarction is highlighted by C5b-9 stain -E- and alkaline phosphatase -F-. The area of infarct is located in the center of a fascicle, and is composed of back-to-back, rather than scattered, necrotic fibers.
-left- Anti-Mi-2 titer strongly correlates with serum CK -r=0.96; p=0.002- and degree of myofiber damage.
-right- Anti-NXP-2 titer does not correlate with serum CK -r=-0.21; p=0.49-.
To cite this abstract in AMA style:
Nguyen M, Do V, Yell P, Jo C, Liu J, Wright T, Cai C. Myositis-Specific Antibodies and Muscle Histopathology in Juvenile Dermatomyositis: New Insights into the Mechanism of Injury [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/myositis-specific-antibodies-and-muscle-histopathology-in-juvenile-dermatomyositis-new-insights-into-the-mechanism-of-injury/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/myositis-specific-antibodies-and-muscle-histopathology-in-juvenile-dermatomyositis-new-insights-into-the-mechanism-of-injury/