Session Information
The 2020 Pediatric Rheumatology Symposium, originally scheduled for April 29 – May 2, was postponed due to COVID-19; therefore, abstracts were not presented as scheduled.
Session Type: Poster Breakout Session
Session Time: 5:10PM-5:40PM
Background/Purpose: The presence of myositis specific autoantibodies (MSA) and myositis associated antibodies (MAA) has been associated with specific clinical phenotypes, various organ involvement and disease prognosis in both children and adults with idiopathic inflammatory myopathies (IIM). Despite the growing literature surrounding MSA/MAA in patients with IIM, the majority of studies include predominantly white populations with limited data on the extent to which race and ethnicity impact disease manifestations, treatment response and long-term clinical outcomes. We performed a retrospective case series of pediatric patients with IIM to determine MSA/MAA prevalence, clinical phenotype, disease course and treatment response in a racially diverse population.
Methods: Patients age 2-21 years with a diagnosis of juvenile dermatomyositis (JDM), juvenile polymyositis (JPM) or overlap myositis, who had been tested for MSA/MAA, were eligible for study inclusion. Clinical and laboratory data was collected retrospectively via manual chart review of the electronic medical record. Descriptive statistics were performed to summarize each variable. Given the small sample size, non-parametric testing was performed using Fischer’s exact test, Wilcoxon rank sum test and Kruskal-Wallis test.
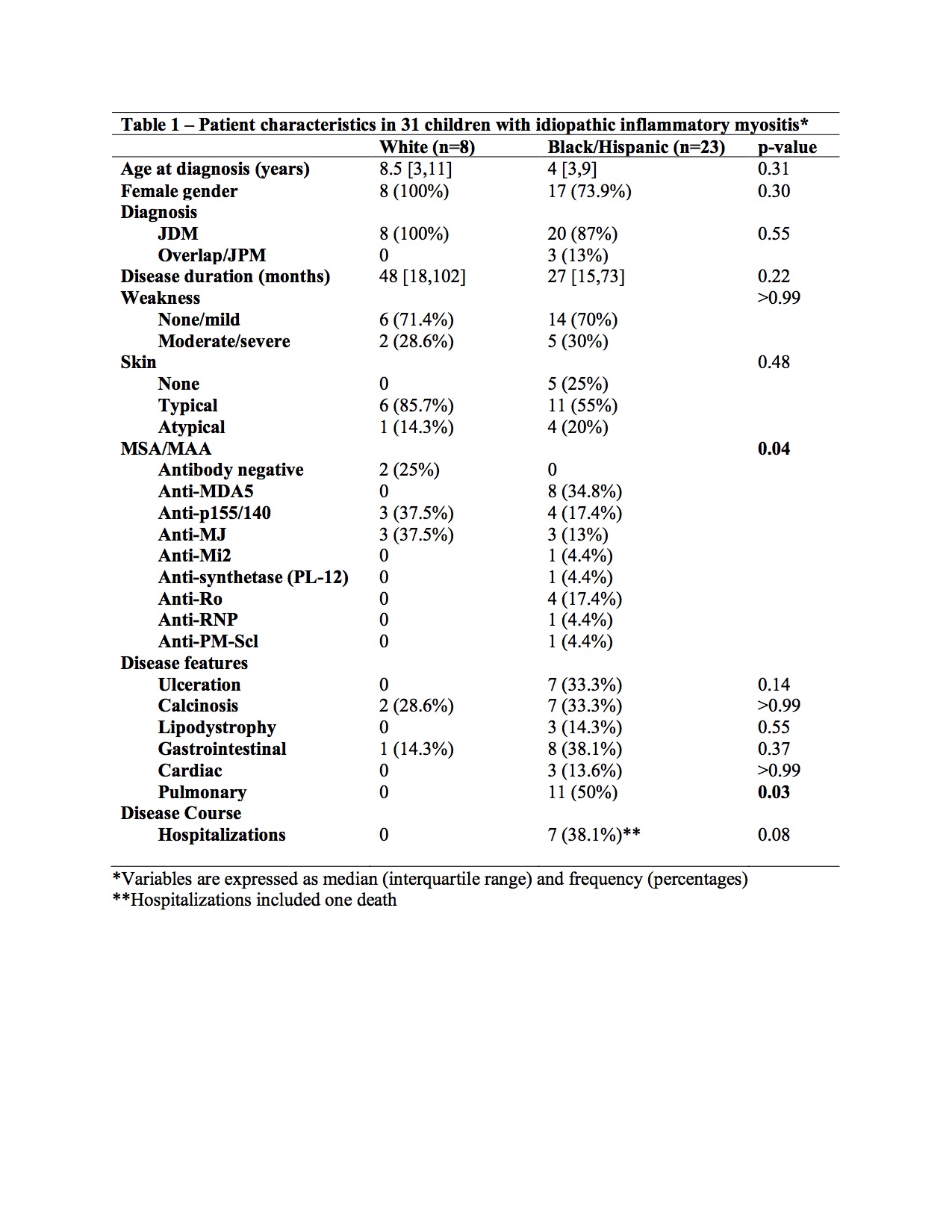
Results: 31 patients were included in the analysis. Overall median age of diagnosis was 7 years (range 2-16), with the majority of female gender (80.7%). Race and ethnicity were self-reported as 48.4% Hispanic, 25.8% White, non-Hispanic, and 25.8% Black, non-Hispanic. The most prevalent MSAs were anti-MDA5 (25.8%), anti-p155/140 (22.6%) and anti-MJ (19.4%), followed by anti-Mi2 (3.2%), anti-synthetase (3.2%) and several overlap autoantibodies. Patient demographics and disease features, grouped by race, are shown in Table 1. Presence of autoantibodies (p=0.04) and pulmonary disease (p=0.03) were significantly higher in patients of Black/Hispanic descent. Although not statistically significant, male gender, cutaneous ulceration, hospitalizations and one death were also only reported in the group of patients with Black/Hispanic descent. Interestingly, there was a relatively high proportion of patients with anti-MDA5 antibodies in our cohort (n=8) and all were of Black/Hispanic descent. As expected, patients with anti-MDA5 antibodies were more likely to have cutaneous ulceration (p=0.02). Of the 11 patients with pulmonary involvement, 5 had anti-MDA5 antibodies (p=0.24).
Conclusion: This study demonstrates a wide variety of MSA/MAA in a racially diverse group of patients with juvenile IIM and further delineates clinical phenotype and disease complications in these groups. Given the rarity of IIM in children, we found a relatively high proportion of children with anti-MDA5 antibodies and have described potentially worse clinical outcomes in children of Black/Hispanic descent. Further investigation is warranted to examine these findings in a larger sample of patients.
To cite this abstract in AMA style:
Wahezi D, Vasquez Canizares N, Tarshish G, Colwell M. Myositis Autoantibodies in a Racially Diverse Population of Children with Idiopathic Inflammatory Myopathies [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 4). https://acrabstracts.org/abstract/myositis-autoantibodies-in-a-racially-diverse-population-of-children-with-idiopathic-inflammatory-myopathies/. Accessed .« Back to 2020 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/myositis-autoantibodies-in-a-racially-diverse-population-of-children-with-idiopathic-inflammatory-myopathies/