Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Systemic sclerosis (SSc) related pulmonary hypertension (PH) carries a high mortality and patients with SSc-PH related to restrictive lung disease having an even worse prognosis. Speculation regarding the potential of MMF to exert anti-fibrotic and anti-remodeling effects on parenchymal lung and vascular intimal fibrosis, led us to query the possible differences in outcomes and survival between 4 groups based on forced vital capacity (FVC) and use of MMF in SSc PH.
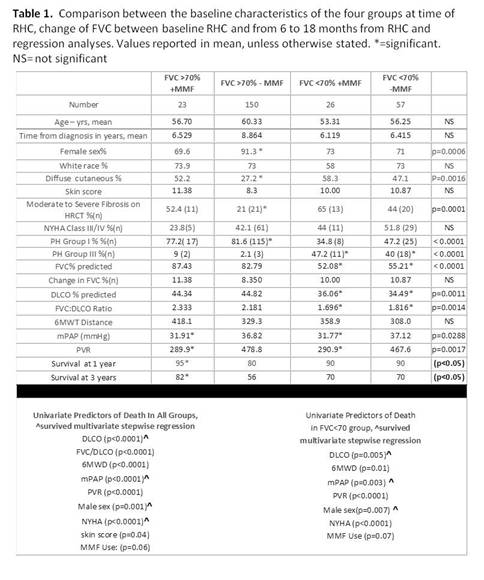
Methods: PHAROS is a prospective registry designed to provide substantive data to recognize aspects of PH unique to SSc. For this analysis patients were stratified by an FVC of >70% or ≤ 70% predicted on spirometry at the time of PH diagnosis by right heart catheterization (RHC ) and then by MMF use greater than 6 months after the diagnosis of PH. Cyclophosphamide use was exclusionary to all groups. Calculations are derived from one-way ANOVA with Tukey’s post test or Kruskal Wallis with Dunn’s post-test. Categorical variables were compared with Chi square. These analyses were followed by Cox and stepwise backward regression analysis to assess baseline characteristics associated with risk of death and Kaplan-Meyer analysis.
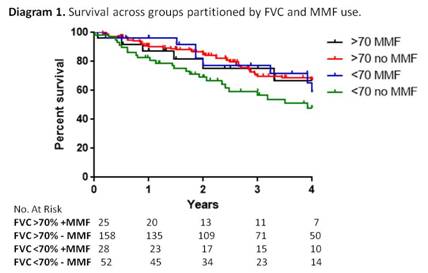
Results: 256 cases from the PHAROS database matched criteria and had baseline spirometry results coincident with diagnostic RHC, of those 173 had a baseline FVC of >70% with 23 on MMF and 150 without; and 83 had a baseline FVC≤70% with 26 on MMF and 57 without. Across groups, no differences were found in age, disease duration, racial distribution nor surprisingly in skin score, 6 minute walk test for distance or NYHA Class. No detectable differences were found between groups in 6-18 month interval change from baseline FVC% in MMF- groups or from post-RHC initiation of MMF in the MMF+ groups. Of interest, baseline mPAP and PVR were lower in both MMF+ groups regardless of FVC. Though survival is numerically worst with FVC<70 without MMF at 4 years, it did not quite reach statistical significance in Kaplan-Meier analysis at 4 (p=0.06) or 3 years (p=0.08). Survival for both MMF groups was between 70% and 82% but only 56% for the patients with a low FVC not treated with MMF. Male sex was a significant independent predictor of death in all groups especially when FVC was <70%.
Conclusion: The trend for improved survival in patients with PH with FVC <70 who were treated with MMF even in the absence of improvement of FVC is intriguing. Whether it has an effect on pulmonary artery remodeling should be considered. These findings warrant prospective controlled investigations of MMF in SSc PH particularly in those with restrictive lung disease.
Disclosure:
L. A. Saketkoo,
None;
M. R. Lammi,
None;
A. Fischer,
Actelion Pharmaceuticals US,
5,
Gilead Sciences,
5,
InterMune,
5,
Gilead Sciences,
8;
J. A. Molitor,
UCB,
2,
Actekion,
2;
V. D. Steen,
Actelion Pharmaceuticals US,
8,
United Therapeutics,
5,
Gilead Science,
8,
Roche Pharmaceuticals,
2,
Sanofi-Aventis Pharmaceutical,
2,
CSL Berhing,
2,
Intermune,
2,
Bayer,
5.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/mycophenolate-mofetil-mmf-use-in-scleroderma-patients-with-pulmonary-hypertension-observations-from-the-pulmonary-hypertension-assessment-and-recognition-of-outcomes-in-scleroderma-cohort/