Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose:
Nephritis (LN) in pediatric systemic lupus erythematosus (pSLE) requires treatment (tx) with corticosteroids (CS) and other agents such as mycophenolate mofetil (MMF) or cyclophosphamide (CYC). However, some patients (pts) fail standard therapy leaving physicians with few options. Although a recent phase II randomized controlled combination trial of abatacept and MMF (ABA+MMF) in adult SLE did not meet its endpoints, we examined if this combination therapy may have a therapeutic benefit in pSLE pts with refractory LN.
Methods:
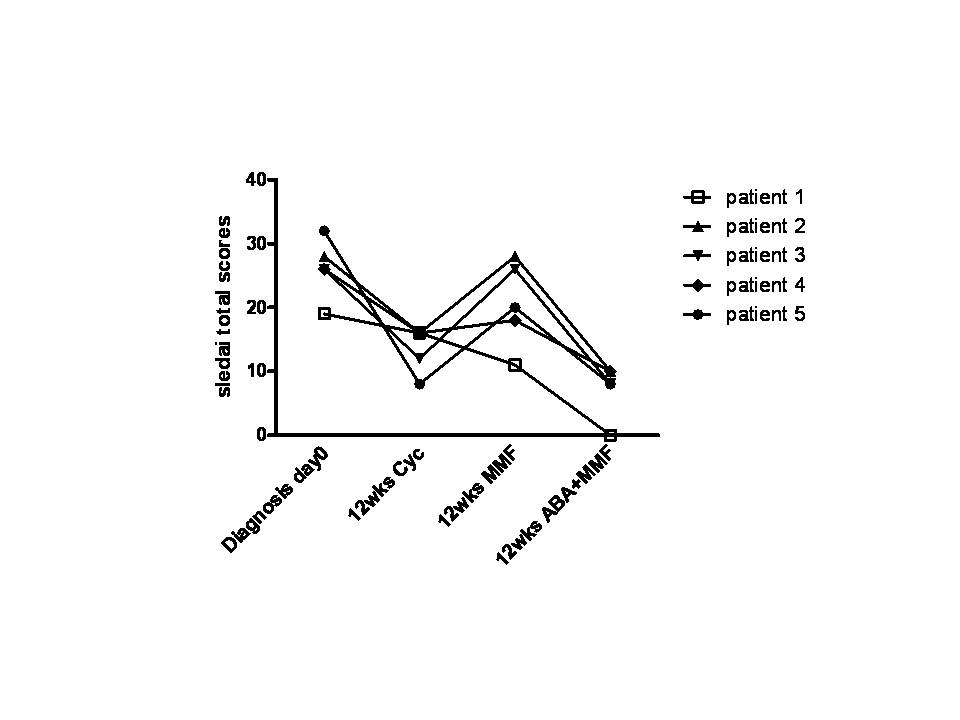
We performed a retrospective observational study in 5 pSLE pts with class IV and V lupus nephritis. All pts were treated with ABA+MMF after previous treatment and failure or intolerance to CYC and MMF with concomitant CS. Data collected included demographics, disease duration, renal histology and medications used. SLE Disease Activity score (SLEDAI) including parameters of systemic and renal disease activity were assessed at baseline and after 12 weeks of each tx.
Results:
Pt age at diagnosis was 9-15years (mean 12.6 ± 2.3). Average disease duration was 22-97 months (mo) (mean 52.8 ± 30.8), before ABA+MMF therapy was started. Two pts had class IV, 1 pt had class V and 2 pts had class IV/V LN.
All 5 pts had a statistically significant decrease in their SLEDAI scores and successfully had their steroid dose reduced while on ABA+MMF. One pt achieved complete remission and 3 pts were completely weaned off steroids after an average of 9 mo (3-16mo). Repeated ANOVA analyses comparing SLEDAI scores at baseline and after 12 weeks of CYC, MMF and ABA+MMF respectively, showed a statistically significant pattern of change from the baseline score with each change in therapy (P<0.0001). Paired comparison of SLEDAI scores on each drug to baseline scores showed the most significant improvement with combination therapy (MMF+ABA p=0.0001, CYC p=0.0199, MMF p=0.0520).
Conclusion:
The above data suggests that combination therapy with ABA+ MMF can be superior to MMF alone and may be an effective option in refractory pSLE nephritis, raising the possibility of a synergistic effect between the two drugs. Additional studies are needed in pSLE to further assess the efficacy of this combo tx.
Disclosure:
R. Castillo,
None;
S. M. Radhakrishna,
None;
A. O. Reiff,
None;
K. A. Marzan,
None.
« Back to 2012 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/mycophenolate-mofetil-and-abatacept-combination-therapy-in-refractory-pediatric-systemic-lupus-erythematosus-nephritis/