Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: The COVID-19 pandemic led to rapid expansion of telemedicine in all fields, including rheumatology. We hypothesized that increased use of telemedicine would reduce no-show visits, given greater convenience and reduced barriers such as travel or transportation, which could also potentially reduce disparities in visit attendance.
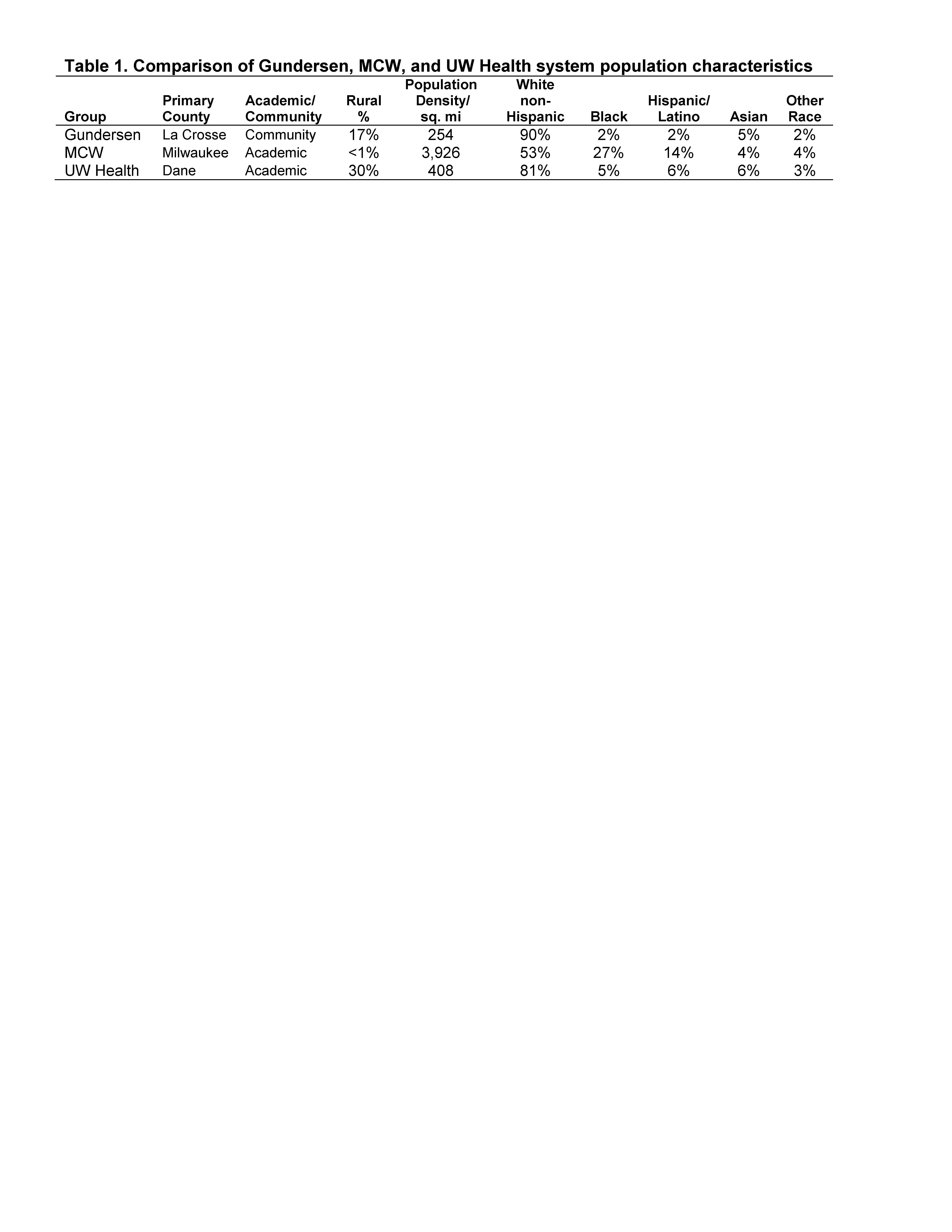
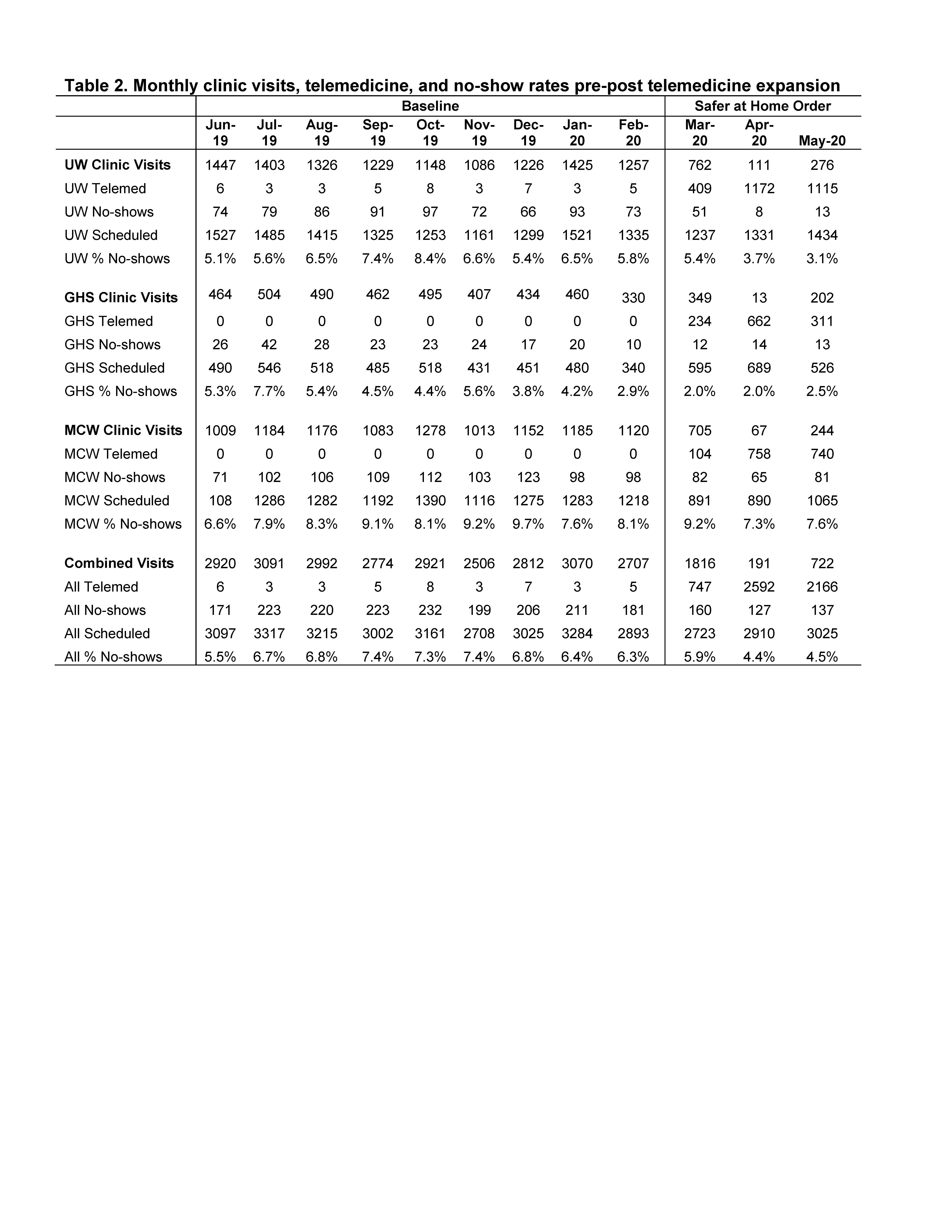
Methods: We conducted an observational study with three rheumatology groups in one state (Table 1) serving diverse academic urban (Medical College of Wisconsin-MCW in Milwaukee), suburban (University of Wisconsin-UW in Madison), and community populations (Gundersen Health System-GHS in Lacrosse). To compare rates of no-shows before and after a statewide safer at home order 3/26-5/26/2020, electronic health record (EHR) data were queried for monthly rates of in-clinic visits, telemedicine visits, and no-show counts across one year, 6/1/2019-5/31/2020. Telemedicine included scheduled telephone or video encounters versus in-person clinic visits; most were via telephone. No-show rates were defined as the proportion of visits that did not successfully reach a patient divided by the total number of scheduled clinic or telemedicine visits. Chi square calculations compared no-shows and completed visits before and after March 2020 at each site and combined. The project was exempted by local IRBs.
Results: At baseline, only one center used telemedicine with a mean of five visits per month. In March 2020, telemedicine visits increased at all centers. By April, telemedicine outnumbered clinic visits 13-fold, while total volumes remained high (Table 2). Two sites saw no-show rates decline from 4.2-8.4% before to 2.0-5.8% after March 2020. As hypothesized, rates declined in months with higher telemedicine volumes at two centers (Fig 1A & B black lines p< 0.0001). However, declines were not statistically significant at the urban center (Fig 1C). Combined data (Fig 1D) showed declines in no-show rates at the time of telemedicine expansion (p.0001).
Limitations include limited information regarding telemedicine implementation across sites (e.g., live pre-visit reminder calls with telemedicine vs. automated reminders), possible missed no-show visits, and the lack of adjustment in our observational study. Personal interaction via reminder calls from office staff, or the novelty of telemedicine might have also reduced no-show rates and merits further study.
Conclusion: Our findings suggest that in the period of increased telemedicine visits after March 2020, no-show rates decreased while overall total visit volumes remained high. Two centers serving more rural populations showed particular gains in reducing no shows. The urban center did not see reduced no-show rates, potentially predicting ongoing healthcare delivery disparities with telemedicine or a need for more implementation support in urban populations. Future studies should follow longitudinal trends and compare multivariable predictors (e.g., race, age group, travel distance) of no-shows for in-clinic versus telemedicine. Likewise, further work should examine how to optimize telemedicine implementation overall and with vulnerable populations, and how policy can support optimal telemedicine use.
 Figure 1. Total visits, telemedicine visits & no-show encounters by month at three centers and overall combined
Figure 1. Total visits, telemedicine visits & no-show encounters by month at three centers and overall combined
To cite this abstract in AMA style:
Bartels C, Gazeley D, Rosenthal A, Ferguson S, Ramly E, Messina M, White D. Multisite Study of the Impact of COVID-19 Era Telemedicine Expansion on Reduction in No-Show Rates [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/multisite-study-of-the-impact-of-covid-19-era-telemedicine-expansion-on-reduction-in-no-show-rates/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/multisite-study-of-the-impact-of-covid-19-era-telemedicine-expansion-on-reduction-in-no-show-rates/