Session Information
Date: Sunday, November 10, 2019
Title: 3S107: Pediatric Rheumatology – Clinical I: Systemic JIA (915–920)
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Recent experiences suggest a disturbing epidemic of digital clubbing and insidious, Pulmonary Alveolar Proteinosis (PAP)-like lung disease occurring in patients with Systemic Juvenile Idiopathic Arthritis (SJIA-PAP). Many SJIA-PAP patients also suffer from prior and/or concomitant Macrophage Activation Syndrome (MAS) and most have been exposed to IL-1 and/or IL-6 inhibition. Though variable, many SJIA-PAP patients progress to pulmonary hypertension, respiratory failure, and death. To improve diagnostic screening and pathogenic understanding of SJIA-PAP, we undertook a near-proteomic serum analysis in SJIA-PAP and related controls.
Methods: We measured 1311 distinct analytes in 162 serum samples from a cohort of patients with SJIA-PAP (n=11), inactive sJIA/MAS (30, including two NLRC4-MAS), active SJIA (24), active MAS (12, including two NLRC4-MAS), autoimmune/genetic PAP (14), Neonatal-Onset Multisystem Inflammatory Disease (5), STING-associated Vasculopathy of Infancy with interstitial lung disease (4), and healthy controls (21). Targets were measured using Slow Off-rate Modified Aptamers (SOMAmers), augmented by selected Luminex-based measurements. We used a linear regression model (Limma) to identify relationships with individual diseases.
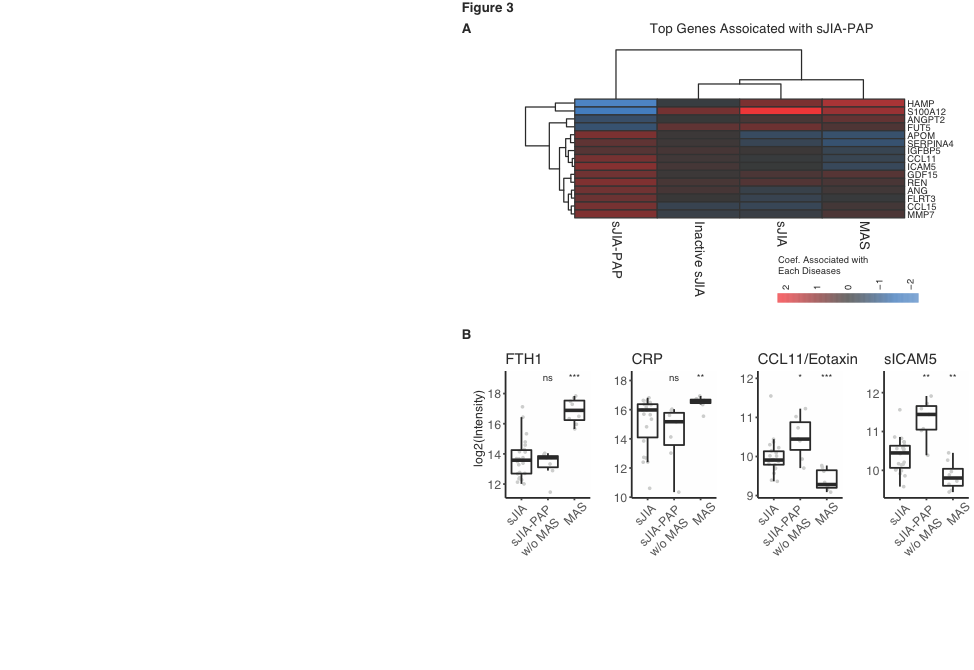
Results: Biomarkers canonically associated with SJIA and MAS (e.g. CRP, S100 proteins, ferritin, IL-18) supported the validity of pre-analysis groupings (Fig. 1). Novel, MAS-specific biomarkers suggested targetable cell death (heat-shock proteins) and metabolic (glycolytic enzyme) pathways (Fig. 2). Analytes elevated in SJIA-PAP but not inactive SJIA, active SJIA, or active MAS (e.g. sICAM-5 & MMP7) suggest lung-intrinsic macrophage activity and may aid in screening or monitoring SJIA-PAP. About half the SJIA-PAP samples demonstrated MAS-like features despite the absence of overt MAS, while the other half displayed relatively low CRP and ferritin levels (Fig 3B), lacked prominent elements of the sJIA/MAS signature (e.g., S100, heat-shock proteins), but had elevated IL-18. Lung disease in these patients was not resolved, and they expressed an sJIA-PAP signature (Fig 3B) that did not correlate with the MAS signature, suggesting distinct regulation of MAS and SJIA-PAP.
Conclusion: This massively-multiplexed serum analysis identified novel targets and pathways in MAS, and suggested an eosinophilic feature in SJIA-PAP patients. High MAS activity was frequently observed despite the absence of overt MAS, but was not required to maintain SJIA-PAP inflammation. Though these data require prospective validation, they provide mechanistic insights into SJIA, MAS, and the development of SJIA-PAP and may provide candidate biomarkers with which to better diagnose and monitor these disorders.
To cite this abstract in AMA style:
Chen G, Schulert G, De Jesus A, Saper V, Schneider C, Trapnell B, Grom A, Goldbach-Mansky R, Mellins E, Khatri P, Canna S. Multiplex Serum Analysis Identifies Potential Biomarkers of Systemic Juvenile Idiopathic Arthritis, Macrophage Activation Syndrome, and Associated Pulmonary Alveolar Proteinosis: Evidence for Independently-regulated Hyperinflammatory and Eosinophilic Inflammation [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/multiplex-serum-analysis-identifies-potential-biomarkers-of-systemic-juvenile-idiopathic-arthritis-macrophage-activation-syndrome-and-associated-pulmonary-alveolar-proteinosis-evidence-for-independ/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/multiplex-serum-analysis-identifies-potential-biomarkers-of-systemic-juvenile-idiopathic-arthritis-macrophage-activation-syndrome-and-associated-pulmonary-alveolar-proteinosis-evidence-for-independ/