Session Information
Date: Sunday, November 5, 2017
Title: Epidemiology and Public Health I: Lung, Bone, and Infection Outcomes
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: In prior work, we found a higher incidence of hip fractures in RA than age and sex matched general population controls (4.1 vs. 2.9 per 1000 PY). To assess burden of disease, we compared age- and sex-adjusted all-cause mortality post hip fracture in RA and general population controls.
Methods: We conducted a retrospective study of a population-based incident RA cohort, using administrative health data. Using physician billing data, we identified all people with RA onset between 1997 and 2009 in a Canadian province. Controls (with no diagnosis of RA or other inflammatory arthritis) were randomly selected from the general population, matched 2:1 to RA cases on birth yr, gender and index yr. RA patients and controls with prior hip fractures, pathological fractures or Paget’s disease were excluded. Hip fractures were identified using hospitalization data (ICD9-CM codes 820.0, 820.2; ICD10-CA codes S72.0, S72.1, S72.2), from ≤25 codes defining reason for admission or complications during hospitalization. RA individuals and controls were followed from incident hip fracture to death, last health care use, or study end (Dec. 2014). Mortality data was obtained from Vital Statistics. Cox-proportional hazard models, adjusted for age and sex, compared mortality risk in RA vs. controls with a hip fracture.
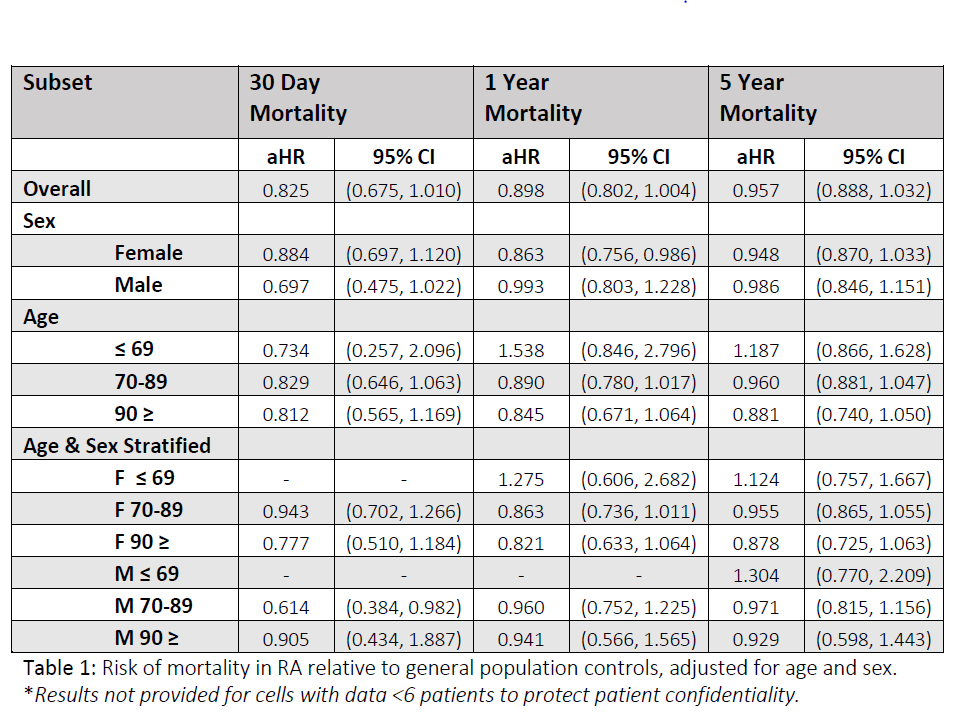
Results: The cohort included 60,101 incident RA cases and 120,462 controls, of whom 2463 (4.1%) RA individuals and 3566 (3.0%) controls sustained an incident hip fracture and make up the study sample (78% females in RA and 81%s in controls; mean (SD) age at time of fracture: 78.9(10.9) yrs for RA and 82.1(9.0) yrs for controls). Crude all-cause mortality rate post hip fracture was 5.9% (n=143) and 8.2% (n=288) at 30 days; and 19.9% (n=481) and 24.5% (n=854) at 1-yr, for RA and controls, respectively. After age and sex adjustment, RA persons with hip fractures had a 17.5% lower risk of death than persons without RA at 30-days and 10.2% lower risk at 1-yr. The mean age at death for 30-day mortality was 83.9 yrs for RA and 86.1 yrs for controls.
Conclusion: Despite a higher incidence of hip fractures in RA, the 30-day and 1-year post hip fracture all-cause mortality was lower in RA than controls, after adjusting for sex and age at time of fracture. Further research is needed to understand whether mortality differences are related to co-morbidities, differences in post-op care, or other characteristics influencing post-fracture mortality risk.
To cite this abstract in AMA style:
Jones CA, Guy P, Xie H, Sayre EC, Lacaille D. Mortality Post Hip Fracture in Rheumatoid Arthritis Compared to General Population Controls, a Population-Based Study [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/mortality-post-hip-fracture-in-rheumatoid-arthritis-compared-to-general-population-controls-a-population-based-study/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/mortality-post-hip-fracture-in-rheumatoid-arthritis-compared-to-general-population-controls-a-population-based-study/