Session Information
Session Type: Abstract Submissions (ARHP)
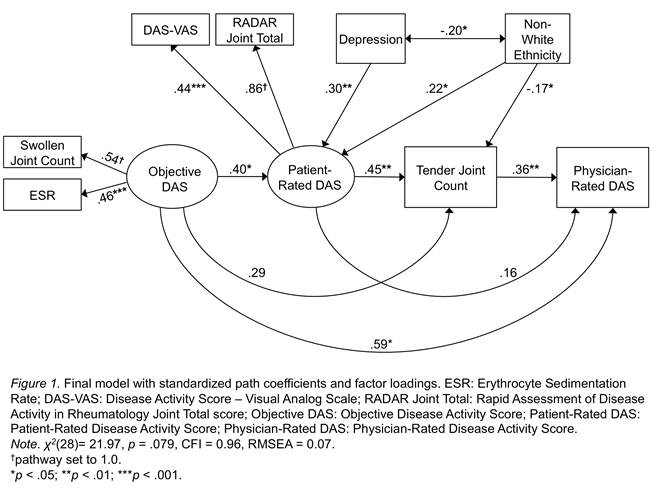
Background/Purpose: The purpose of this study was to examine a multidimensional, integrated model describing the interrelations among rheumatoid arthritis (RA) objective disease activity, patient-rated disease activity, tender joint count, and related psychosocial factors as determinants of physician-rated disease activity (see Figure 1). It was expected that objective disease activity would be positively associated with physician-rated disease activity, both directly and indirectly through the hypothesized mediators of patient-rated disease activity and tender joint count. Methods: The data of 105 participants satisfying the ACR classification criteria for RA were drawn from baseline of a randomized comparative efficacy trial of psychosocial interventions for RA. In the hypothesized model, objective disease activity (DAS-28 Swollen Joint Count and ESR), patient-rated disease activity (Rapid Assessment of Disease Activity in Rheumatology total joint score and disease activity VAS), physician-rated joint tenderness score serve as determinants of physician-rated disease activity. EQS 6.1 was used to evaluate the structural model, and the significance of estimated indirect effects (calculated based on the Sobel method) was taken as evidence of mediation. Results: The hypothesized model fit the data well, χ2(28)= 21.97, p = .079, CFI = 0.96, RMSEA = 0.07, and the specified predictors explained 84% of the variance in physician-rated disease activity (see Figure 1). Greater objective disease activity directly predicted physician-rated disease activity and contributed to higher levels of patient-rated disease activity, which, in turn, predicted a higher tender joint count which ultimately exerted a strong positive effect on physician-rated disease activity. While objective disease activity had a strong direct effect on physician-rated disease activity, partial mediation was established because the strength of this association diminished when the model included the hypothesized predictors (as evidenced by its significant indirect effect; βindirect = .24, p < .001). With regard to patients' self-ratings of RA symptoms, depressive symptomatology and non-white ethnicity were shown as positively associated with higher self-perceived levels of disease activity. In contrast, non-white ethnicity was associated with significantly lower physician-rated tender joint scores. Conclusion: Findings confirmed the importance of a multi-dimensional framework in evaluating RA disease activity and elucidated the mechanisms that perpetuate health disparities. These results identify a specific point in the clinical encounter where an increased awareness of patients’ experiences of their disease can contribute to more accurate ratings and improved outcomes.
Disclosure:
J. R. Ayeroff,
None;
S. R. Ormseth,
None;
D. Hardy,
None;
M. R. Irwin,
None;
M. H. Weisman,
None;
P. M. Nicassio,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/model-examining-factors-related-to-physicians-ratings-of-disease-activity-in-patients-with-ra/