Session Information
Date: Sunday, November 8, 2015
Title: Rheumatoid Arthritis - Small Molecules, Biologics and Gene Therapy Poster I
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatoid arthritis (RA) is associated with reduction of bone mineral density (BMD) and increased risk of peripheral and axial fractures. Methotrexate is the first-line treatment in this disease. MTX has been suspected to play a noxious role on bone of patients treated for leukemia or RA. We aimed to assess the effect of MTX on BMD after 1 year of treatment, in patients with RA.
Methods: We performed a systematic review and a meta-analysis of the literature. Two authors (RK and YD) independently screened PubMed-Medline, the Cochrane library and Ovid journals databases. Key words were: “rheumatoid arthritis” AND “methotrexate” AND (“mineral densityÓ or “remodeling markers” or “formation” or “resorptionÓ or “boneÓ). Data, including BMD variation, were extracted using a predetermined form. We selected all prospective studies, with assessment of baseline and 1-year lumbar spine, femoral neck or hip BMD, in patients treated by methotrexate monotherapy. This screening was supplemented by hand searching of relevant references in selected papers. Studies were limited to those concerning human species, published in English, before March 2015. Pooled BMD variation was computed by meta-analysis.
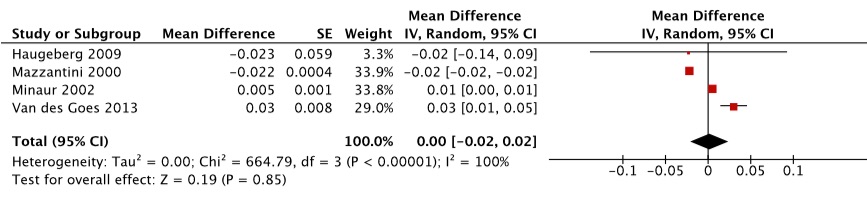
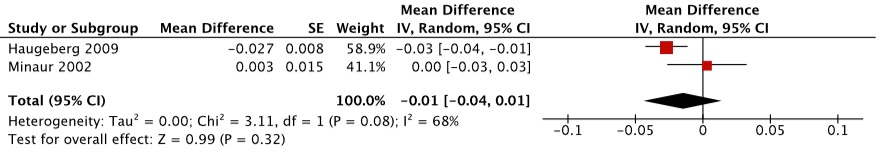
Results: We identified 433 articles in PubMed database and 7 in Cochrane or Ovid databases. We selected 5 eligible references for the systematic review and 4 relevant for meta-analysis. We analyzed 144 patients. 106 were women, 94 displayed early arthritis (<1 year), they had active RA. Two studies included in the meta-analysis contained possibility of bisphosphonates treatment and steroids therapy (Table 1). Meta-analysis concerning 1-year lumbar BMD variation did not show a significant variation: 0.00 g/cm2, 95% confidence interval (95%CI) [-0.02, 0.02] (Figure 1a). Meta-analysis concerning 1-year femoral neck BMD variation showed a non-significant variation: -0.01 g/cm2, 95%CI [-0.04, +0.01] (Figure 1b). Meta-analysis was not possible for 1-year total hip BMD variation. Estimated heterogeneity of studies was high.
Table 1. Main characteristics of the studies included in the meta-analysis
|
Reference |
Study type |
MTX Population |
Age, mean +/- SD |
Disease duration (year) |
Percentage female |
Corticotherapy (Prednisone ³10 mg/day) |
Bisphosphonates |
DAS 28 +/- SD |
|
Van Der Goes, 2013 |
Randomized, placebo-controlled, double-blind |
84 |
52 +/- 13 |
< 1 |
65 |
Yes |
Yes |
3.2 +/- 1.1 |
|
Haugeberg, 2009 |
Randomized, placebo-controlled, double-blind |
10 |
53.1 +/-13.7 |
< 1 |
70 |
Yes |
Yes |
7 +/- 0.9 |
|
Marotte, 2007 |
Case-control |
99 |
53.9 +/- 15.9 |
10.9 +/-8.9 |
79 |
No |
Yes |
5 +/- 1.15 |
|
Minaur, 2002 |
Non- randomized, longitudinal |
28 |
62.6 +/- 8.9 |
6.6 |
79 |
No |
No |
5.27 +/- 1 |
|
Mazzantini, 2000 |
Non-randomized, longitudinal |
22 |
59 +/- 9 |
9 +/- 9 |
100 |
No |
No |
– |
Figure 1a. Lumbar BMD meta-analysis
Figure 1b. Femoral BMD meta-analysis
Conclusion: We did not observed a significant variation of 1-year lumbar and femoral neck BMD in patients treated by MTX, thus suggesting a neutral effect of MTX on BMD in RA.
To cite this abstract in AMA style:
Koch R, Barnetche T, Ruyssen-Witrand A, Cantagrel A, Constantin A, Degboé Y. Methotrexate Does Not Influence 1-Year Bone Mineral Density in Rheumatoid Arthritis: A Systematic Review and Meta-Analysis [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/methotrexate-does-not-influence-1-year-bone-mineral-density-in-rheumatoid-arthritis-a-systematic-review-and-meta-analysis/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/methotrexate-does-not-influence-1-year-bone-mineral-density-in-rheumatoid-arthritis-a-systematic-review-and-meta-analysis/