Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Methotrexate (MTX) is a commonly used drug for inflammatory joint diseases. Occasionally, its use has been associated with diffuse interstitial lung disease (DILD) development1. A systematic review (SR) has been carried out using the PRISMA methodology2 in order to determine the extent of involvement of MTX in DILD development in patients with rheumatoid arthritis (RA), psoriatic arthritis (PsA), psoriasis (Pso), juvenile idiopathic arthritis (JIA) or Crohn’s disease-associated arthritis (CD-A).
Methods: Regarding the study selection, eligible studies were SR of randomized controlled trials (RCTs) with/without meta-analysis, RCTs, cohort studies, case-control studies and abstracts with relevant content, published from the year 2008 onwards, with adult population (≥18 years, except in JIA studies) diagnosed with any of the aforementioned pathologies and treated with MTX. The outcome was the onset/exacerbation of DILD.
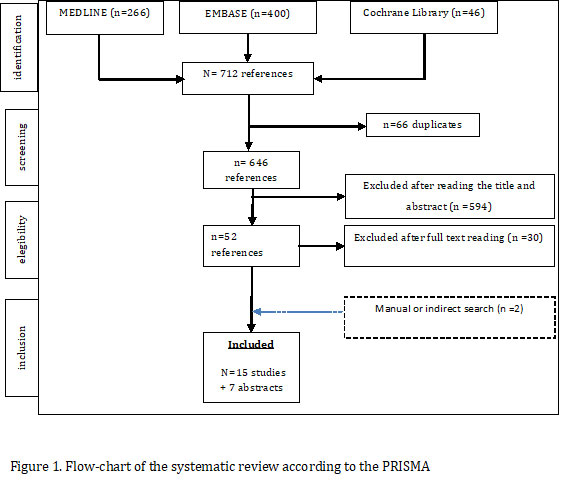
The search and selection of studies for the SR was performed in Medline, Embase and Cochrane, as well as among conference abstracts. Quality assessment and grading of the level of evidence was performed using SIGN3.
According to the attached flow chart (Figure 1), 712 documents were initially retrieved. After full-text selection 15 studies of interest were identified. A meta-analysis was ruled out due to the heterogeneity of the papers.
Results: RA: Conway 20154 evaluated the relative risk (RR) of DILD/RA in patients treated with MTX, and detected a small increase in pneumonitis cases among these patients . Rojas-Serrano 20175 prospectively evaluated the role of MTX in a RA/DILD cohort, and observed better survival in the MTX cohort. England 20186 assessed the association of MTX with mortality risk in patients with/without lung diseases in a large RA cohort, and found no statistical significance. Kiely 20197 performed a multivariate analysis on two early RA cohorts, and found no association between MTX and RA/DILD development; on the contrary, MTX may delay DILD development.
PsA, Pso and CD-A: Conway 20154 found no association between MTX and RR of respiratory adverse events, respiratory infections, or non-infectious respiratory events. Cabello-Zurita 20178 retrospectively evaluated the overall safety related to MTX in a cohort of patients with Pso without finding strong associations with any type of respiratory event.
JIA: Leiskau 20129 performed a retrospective analysis on the influence of cumulative MTX dose and its impact on respiratory function tests or the onset of new long-term respiratory events without finding any association. Alkady 201210 conducted a case-control study evaluating cardiopulmonary evolution in children with asymptomatic JIA. Impairment of lung function parameters was inversely correlated to longer MTX use.
Conclusion: The analysed studies offer no data to establish an association between the use of low-dose MTX and DILD onset in patients with inflammatory diseases. The association of MTX with recurrent acute episodes of previously established lung disease has also not been confirmed.
To cite this abstract in AMA style:
Rubio E, Muñoz A, Casamira N. Methotrexate and Interstitial Lung Disease in Patients with Inflammatory Articular Disease: A Systematic Review [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/methotrexate-and-interstitial-lung-disease-in-patients-with-inflammatory-articular-disease-a-systematic-review/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/methotrexate-and-interstitial-lung-disease-in-patients-with-inflammatory-articular-disease-a-systematic-review/