Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Immunosuppressive medications generally predispose patients to greater risk of serious complications upon COVID-19 infection. This study was initiated to assess whether individual drugs may limit the efficacy of vaccination and predispose to breakthrough infection.
Methods: All patients followed at SUNY Upstate Medical University who has received at least one dose of COVID vaccine (Moderna or Pfizer or Johnson & Johnson) between 1/2020 and 12/2021 were included. Breakthrough infection was determined by positive COVID-19 PCR at 2 weeks or later following vaccination. Patient not on systemic immunosuppression were compared with patients on systemic immunosuppression. Patients on single immunosuppression were compared with patients on no systemic immunosuppression. Chi-square test was performed for statistical analysis.
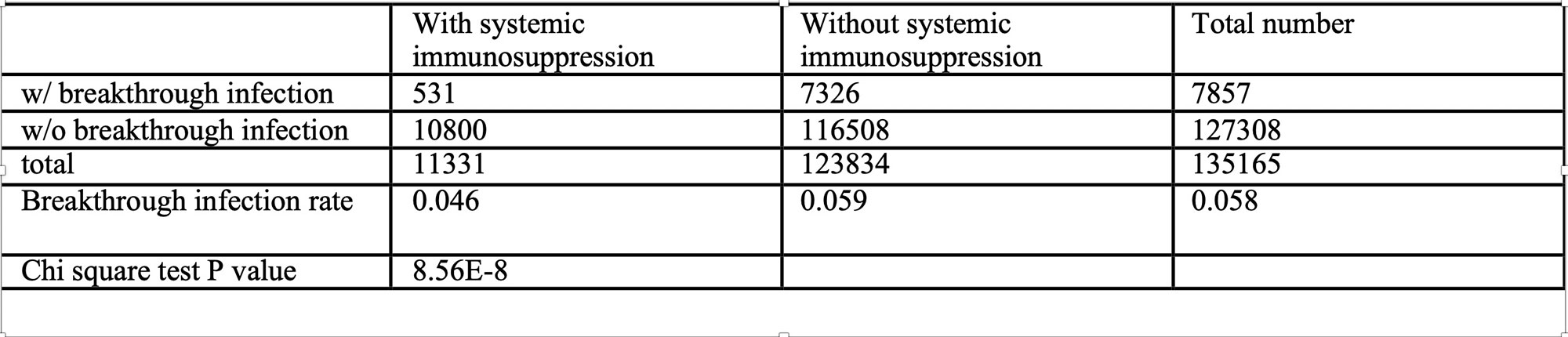
Results: Total 135165 patients were identified to have received at least one dose of COVID vaccine, among those 7857 had breakthrough infection, which is 5.8%. 11331 patients were on systemic immunosuppression (can be single or multiple), and 531 of them developed breakthrough infection, which is 4.6%. 123834 patients were not on any systemic immunosuppression, and 7236 of them developed breakthrough infection, which is 5.9%. The difference is significant with p = 8.56E-8.
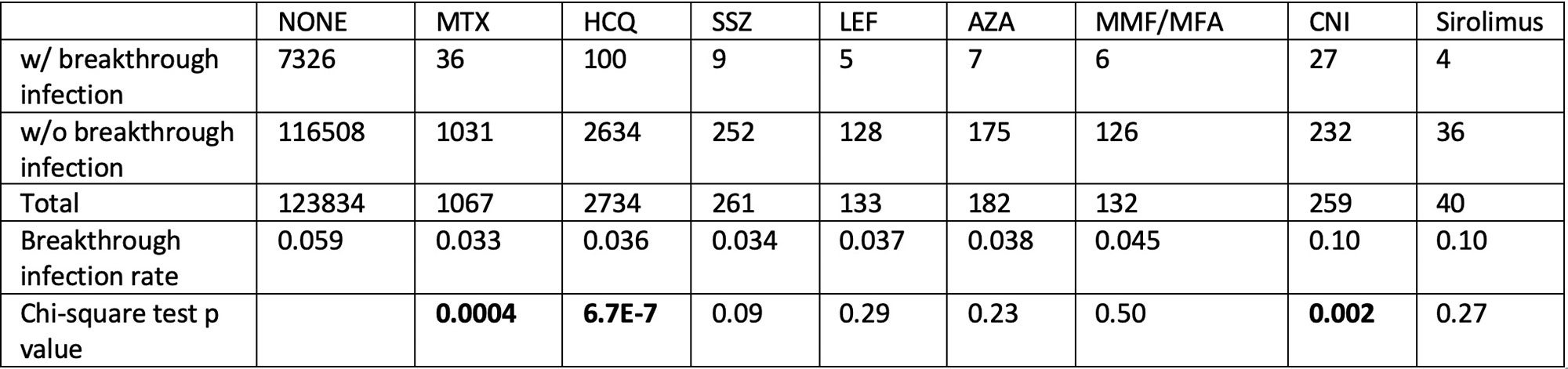
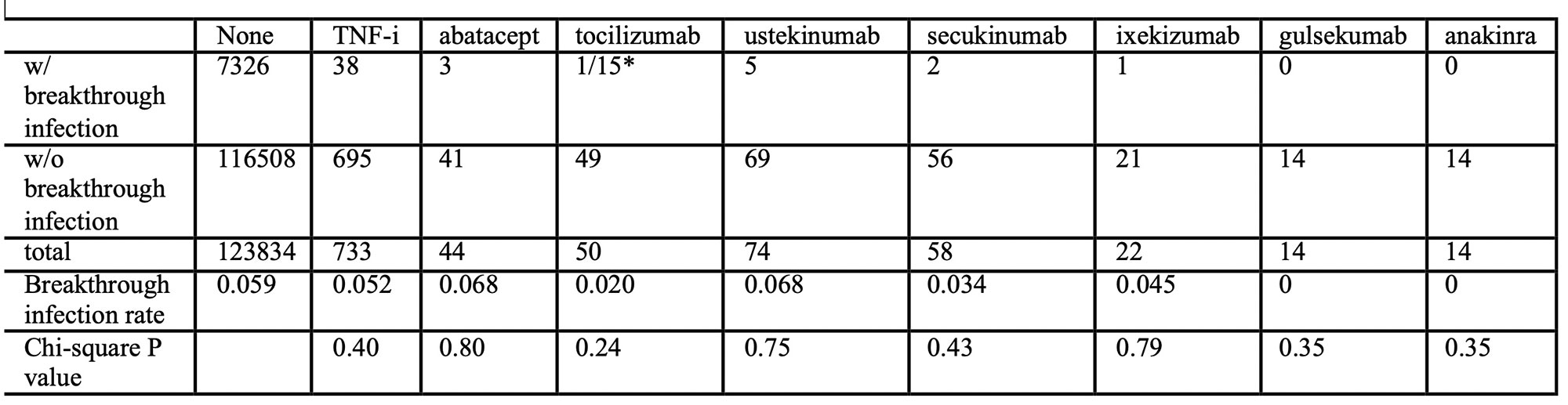
We further compare patients without systemic immunosuppression to patients on only one immunosuppression to see if there is a difference among single immunosuppressive medication. Most immunosuppression when used as single agent didn’t change the breakthrough infection significantly including synthetic DMARDs and biologics. Surprisingly, hydroxychloroquine and methotrexate when used as single agent is associated with a significant lower risk of breakthrough infection. Calcineurin inhibitor (cyclosporin/tacrolimus) was the only immunosuppression associated with significant increase risk of breakthrough infection when used as single agent. All biologic studied here didn’t show any significant increased risk of COVID-19 breakthrough infection.
Conclusion: To our surprise, most immunosuppression when used as single agent didn’t make a significant change in breakthrough infection rate. Methotrexate and hydroxychloroquine used as single agent lowered the risk of breakthrough infection. Calcineurin inhibitors were the only immunosuppressants found to increase the risk of breakthrough infection. This study suggests that immunosuppressive medications did not compromise vaccine protectionLimitationWe did not evaluate if breakthrough infection was severe, mild or asymptomatic. Some patients may have had breakthrough infection but were asymptomatic and didn’t get tested for PCR which will then didn’t get counted. We were also assuming that all patients were exposed to COVID-19 at the same level and using the same precautionary measures. It is very possible that patients on immunosuppression exercise caution which led to less exposure of COVID-19. Lastly, we were only looking at patients with single systemic immunosuppression, combination of immunosuppressants may more likely increase the risk of breakthrough infection. Biologics used in combination with HCQ were not evaluated in this study.
*Total 15 patients on tocilizumab were found to have breakthrough infection, but tocilizumab was used as COVID 19 treatment in 14/15 of them.
To cite this abstract in AMA style:
Wang H, Perl A. Methotrexate and Hydroxychloroquine Used as Single Agent May Diminish Breakthrough Infection After COVID-19 Vaccination [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/methotrexate-and-hydroxychloroquine-used-as-single-agent-may-diminish-breakthrough-infection-after-covid-19-vaccination/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/methotrexate-and-hydroxychloroquine-used-as-single-agent-may-diminish-breakthrough-infection-after-covid-19-vaccination/