Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Despite the pivotal role hydroxychloroquine (HCQ) plays in treating SLE, less than 50% of patients take HCQ as prescribed. Nonadherence versus lack of effect to HCQ are difficult to distinguish, underscoring the importance of measuring HCQ blood levels to assess adherence. Despite this, information and consensus on the clinical impact of incorporating routine testing of HCQ blood levels is lacking. Therefore, we systematically reviewed publications examining the correlation between 1) HCQ levels and adherence, and 2) HCQ levels and SLEDAI scores, in SLE patients. We hypothesized that low HCQ levels would correlate with nonadherence and higher SLEDAI scores.
Methods: A comprehensive search was performed using MeSH heading and keywords in Medline, Embase, CINHL and Web of Science databases. We selected observational and interventional studies that measured HCQ levels and assessed adherence and/or SLEDAI scores in adults with SLE. Newcastle Ottawa Scale and Cochrane Collaboration Risk Assessment tools were used to rate the quality of observational and intervention studies, respectively. We used Forest plots to compare pooled estimates (95% CI) of correlations between HCQ levels and patient or physician reported nonadherence and SLEDAI scores. Heterogeneity was assessed using I2.
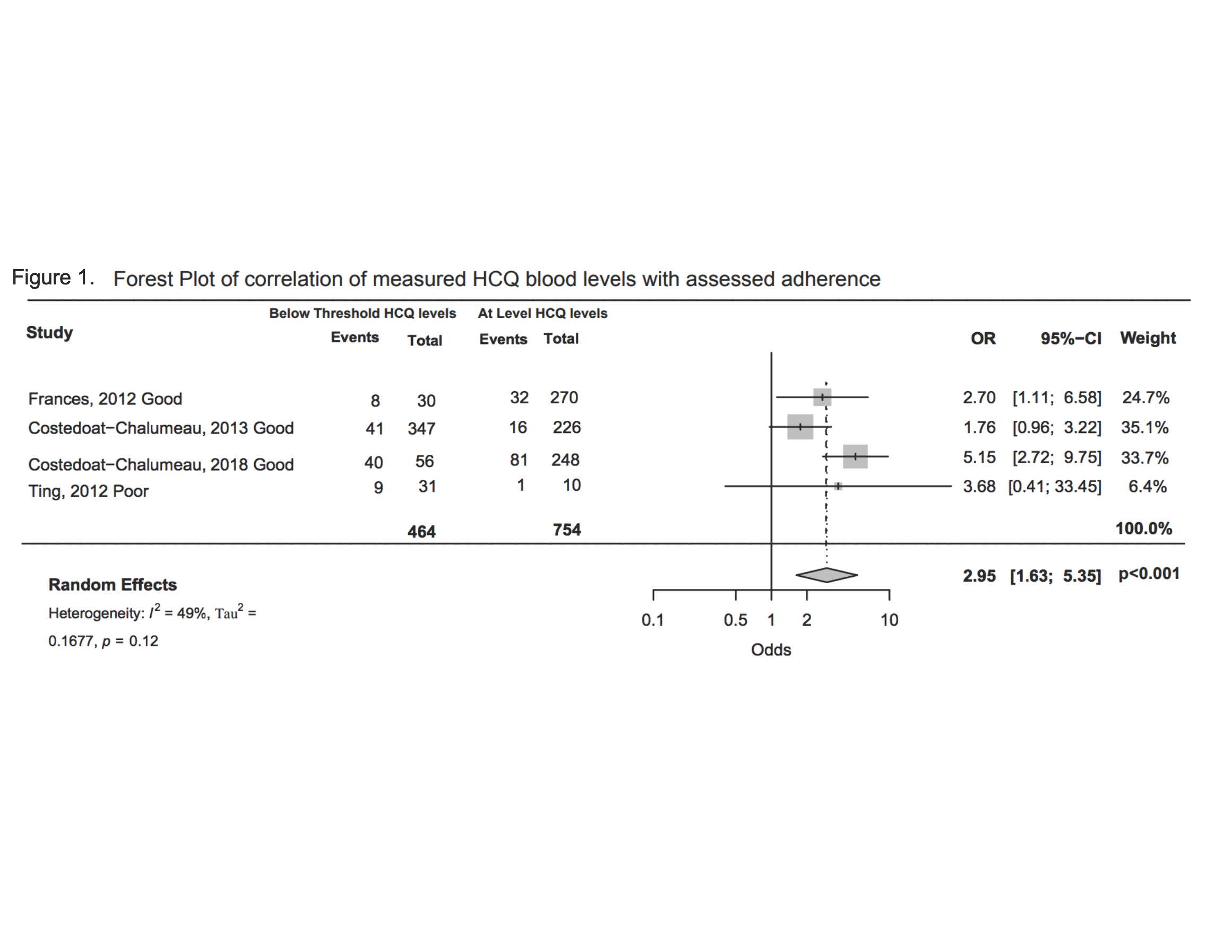
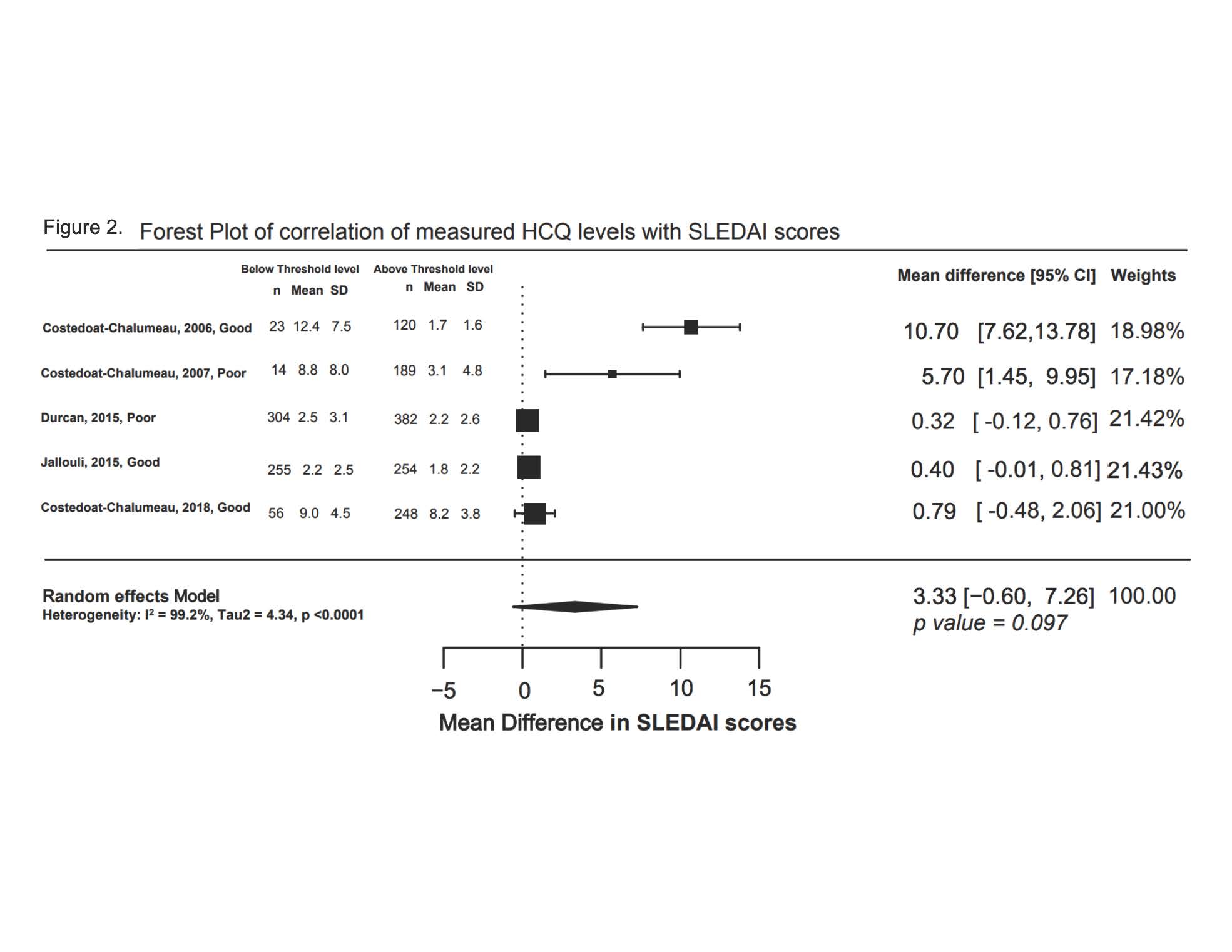
Results: From 306 manually reviewed abstracts, four studies analyzing correlation between HCQ levels and adherence, and five studies examining the correlation between SLEDAI and HCQ blood levels, met inclusion criteria. The odds of nonadherence measured by physician or reported by the patient was 3 times higher in patients with below threshold HCQ blood levels, compared to those with higher HCQ blood levels (OR 2.95, 95% CI 1.63, 5.35, p < 0.001, I2 49%) (Figure 1). The mean SLEDAI score was 3.33 points higher in groups with HCQ levels below threshold levels, but this trend was not statistically significant (δ3.33, 95% CI -0.60, 7.26, p=0.097, I2 99%) (Figure 2). Risk of bias assessment revealed three poor quality studies which were excluded in sensitivity analysis; results remained unchanged. Limitations of our analysis include study heterogeneity and lack of consensus on optimal blood HCQ levels.
Conclusion: We found a good correlation between HCQ levels and non-adherence. While patients with low HCQ levels had higher SLEDAI scores, the p-value for this finding was not statistically significant. Future studies should clarify optimal blood HCQ levels to control lupus, and then investigate the value of measuring blood HCQ levels in clinical care.
To cite this abstract in AMA style:
Garg S, Unnithan R, Hansen K, Costedoat-Chalumeau N, Bartels C. Meta-Analysis Examining the Clinical Significance of Monitoring of Hydroxychloroquine Levels in SLE [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/meta-analysis-examining-the-clinical-significance-of-monitoring-of-hydroxychloroquine-levels-in-sle/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/meta-analysis-examining-the-clinical-significance-of-monitoring-of-hydroxychloroquine-levels-in-sle/