Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: One-third of individuals who contract COVID-19 develop ‘long COVID’ symptoms that persist after their initial illness. Long COVID can cause fatigue, chronic pain, and respiratory and neurological issues that impair physical function and reduce quality of life. Characterization of existing care patterns among long COVID patients is needed to inform development of long COVID care services. Underlying health conditions like rheumatic diseases (RDs) increase long COVID risk, with 37% of RD patients reporting consistent symptoms at 6 months. As long COVID symptoms often overlap with RD symptoms, diagnosing and managing long COVID in this population poses unique challenges. We aimed to describe care pathways and care coordination challenges for patients with rheumatic diseases and long COVID.
Methods: We used electronic medical record (EMR) review to identify 16 rheumatology patients at our institution demonstrating symptoms consistent with long-COVID ≥3 months after a confirmed COVID-19 diagnosis. The study team closely read the EMR documents and created patient journey maps summarizing health status, interactions with health care providers, treatments, and decision making over time. We assessed severity of symptoms thought to be associated with COVID-19 using the WHO Clinical Progression Scale (CPS) during hospitalizations and the Post COVID Functional Status (PCFS) scale at other times, and changes in health status over time were visually represented based on changes in the CPS and PCFS on the patient journey maps. Care coordination challenges were documented and described.
Results: Patient characteristics are shown in Table 1. An excerpt from a patient journey map is shown in Figure 1. Three patients were not hospitalized (PCFS 0-3), 9 were hospitalized within 2 weeks of symptom onset (PCFS 0-4, CPS 4-9), and 4 were hospitalized >= 2 weeks after symptom onset (PCFS 0-3, CPS 4-5). Of the 13 hospitalized patients, 3 were readmitted at least once over the next 8 months. Patients often experienced alternating periods of symptom improvement and worsening.
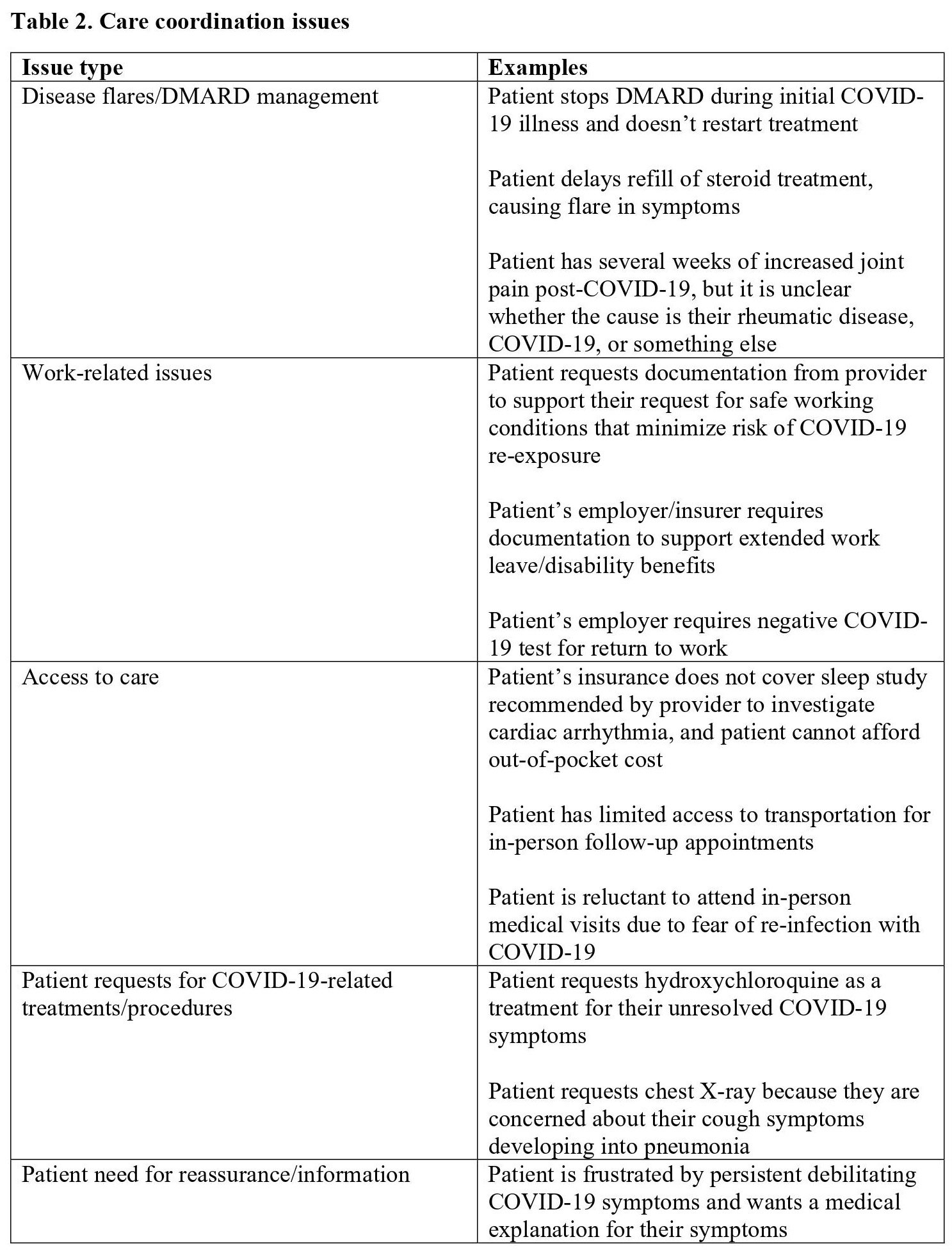
We identified five categories of care coordination issues (Table 2): disease flares/DMARD management, work-related issues, access to care, patient requests for COVID-19-related treatments/procedures, and patient need for reassurance/information.
Conclusion: Among patients with rheumatic disease, cases of long COVID demonstrated variable trajectories and disrupted patients’ functioning and ability to work. In addition to addressing long COVID symptoms, patients relied on assistance from health care providers to submit requests for work leave/return to work. The care coordination issues identified remain broadly relevant at this point in the pandemic, and can be used to establish priorities for research/policy around long COVID both for patients with RMDs and other chronic illnesses.
To cite this abstract in AMA style:
Shaw Y, Wallace B, Chabrier H, Cochrane C, Kim C, Taylor K, Patel A, Keyvan N, Swaroop V, Nguyen N, Hustek S, Moore M, Admon A, Michaud K. Mapping Long COVID-19 Patient Journeys for Rheumatic Disease Patients [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/mapping-long-covid-19-patient-journeys-for-rheumatic-disease-patients/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/mapping-long-covid-19-patient-journeys-for-rheumatic-disease-patients/