Session Information
Session Type: Abstract Session
Session Time: 9:30AM-9:45AM
Background/Purpose: Endothelial proliferation is a key finding in antiphospholipid antibody (aPL)-positive patients with microvascular disease. The mTOR pathway plays a role in the endothelial proliferation leading to aPL-related nephropathy; however, the role of mTOR pathway is not well determined in patients with livedo, which is discolorization of the skin due to reactive dilation of peripheral dermal venules triggered by reduced blood flow in the center. Thus, our primary objective was to investigate mTOR pathway activation in the skin biopsies of aPL-positive patients with livedo reticularis/racemosa.
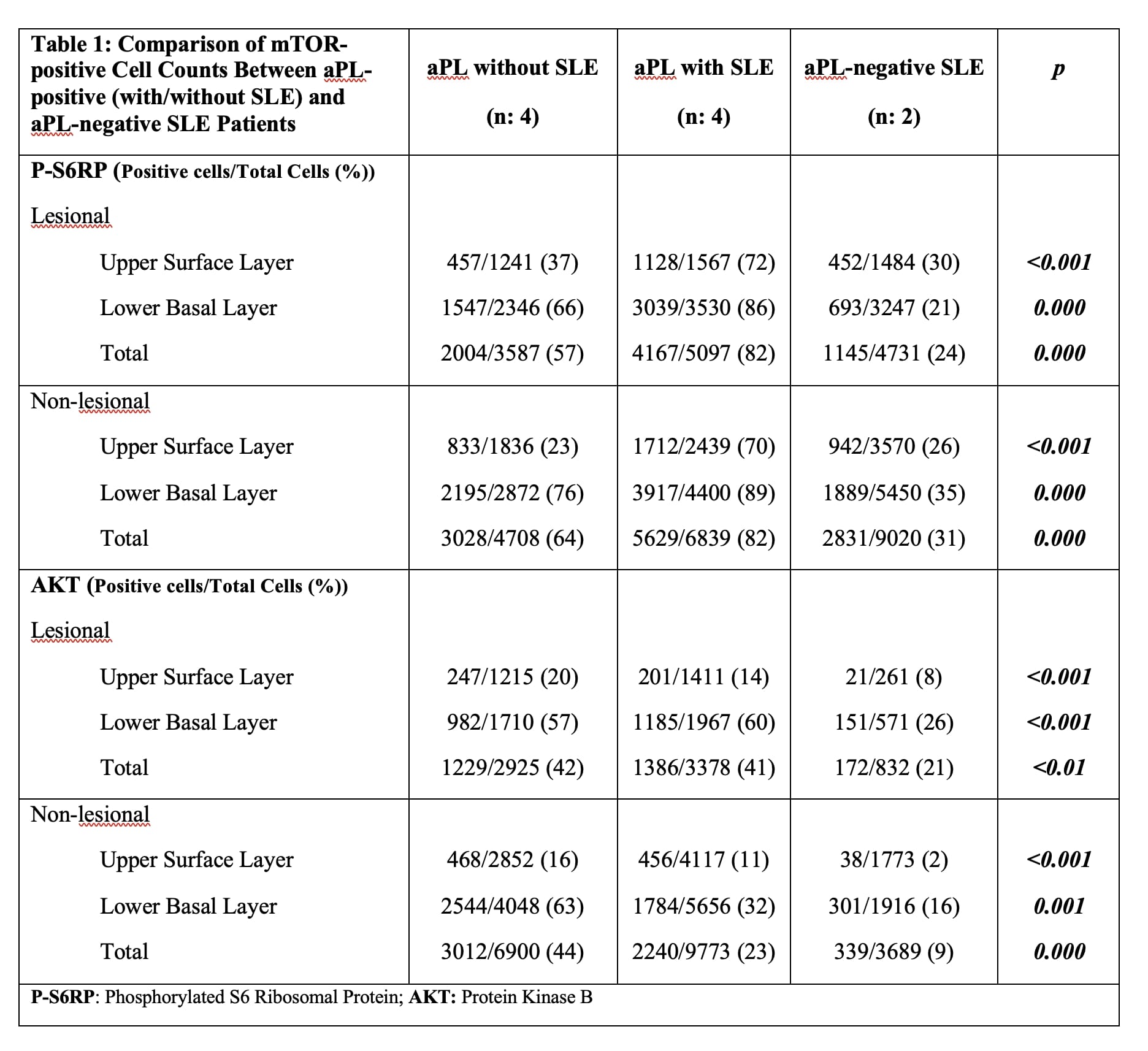
Methods: This cross-sectional study included patients with livedo reticularis/racemosa: a) those with aPL-positivity (LA, aCL IgG/M > 40U, and/or aβ2GPI IgG/M > 40U) with/without systemic lupus erythematosus (SLE); and b) aPL-negative SLE patients as a control group. We collected demographics and aPL-related history. We performed two 5-mm skin biopsies (epidermis) on each patient, one from the erythematous-violaceous peripheral area (lesional) and the second from the non-violaceous central area (non-lesional). Specimens were stained for phosphorylated S6 ribosomal protein (P-S6RP) and protein kinase B (AKT) as a marker of mTOR complex-1 activity. We manually counted cells in the upper superficial and lower basal layers of epidermis and compared the number of cells stained positive for mTOR between different groups (lesional and non-lesional samples in aPL-positive patients vs aPL-negative SLE controls) using chi square test.
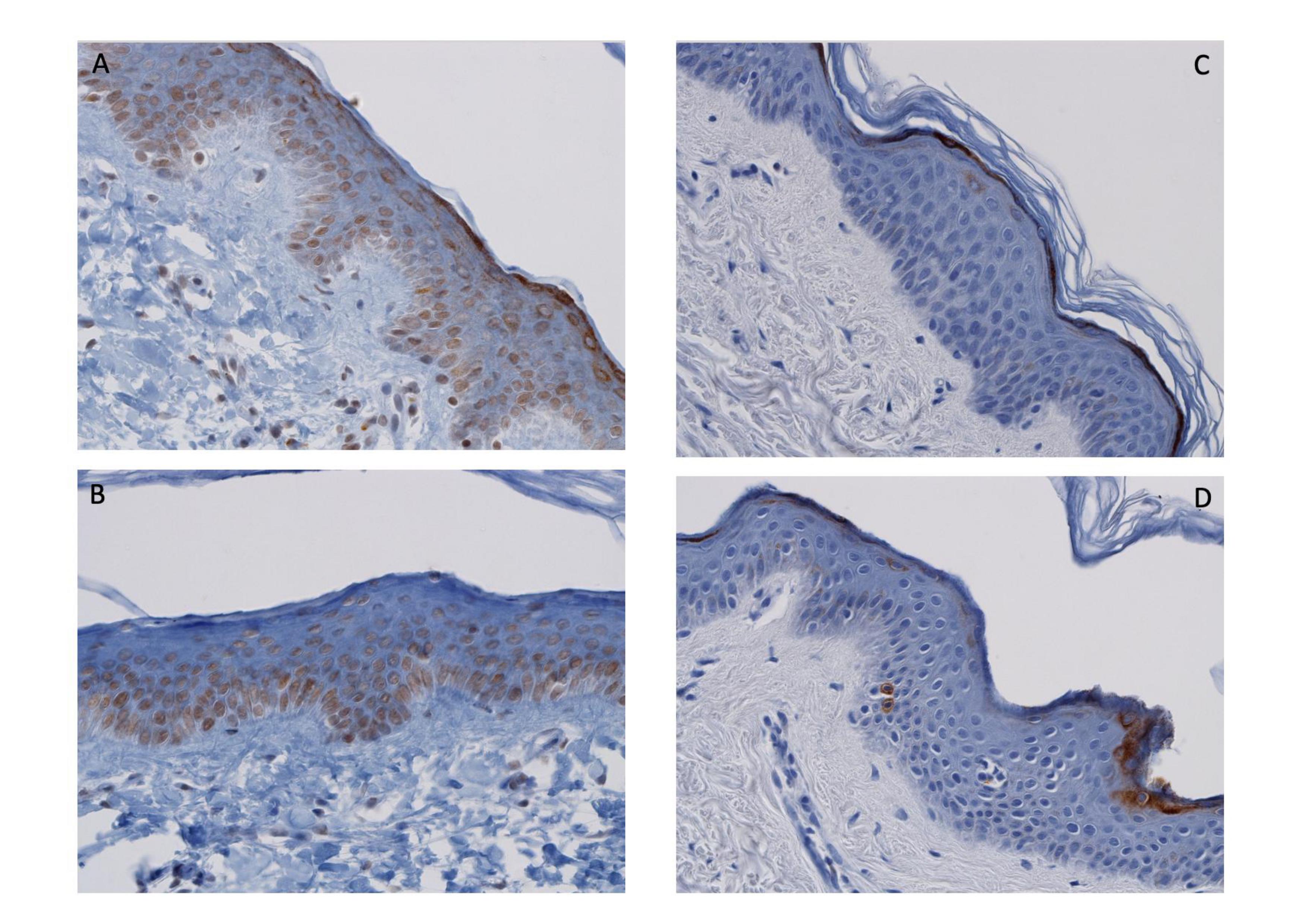
Results: Ten patients were enrolled (aPL-positive without SLE: 4 [APS classification met: 3], aPL-positive SLE: 4 [APS classification met: 3], and aPL-negative SLE control: 2); nine females; all Caucasian; mean age: 45±13.6y. In all aPL-positive patients (n: 8), there was significantly increased mTOR activity in both lesional and non-lesional skin biopsies, compared to the aPL-negative SLE controls (n:2), more pronounced in the lower basal layers (Figure; Table 1). Furthermore, increased mTOR activity in aPL-positive patients was more prominent in the lesional samples, compared to non-lesional (Table 2).
Conclusion: We found increased mTOR activity in livedoid lesions of aPL-positive patients with or without SLE, compared to aPL-negative SLE patients, suggesting there is a role of mTOR pathway activation in aPL-positive patients with livedo. Our results also showed more profound mTOR activity in: a) lower basal layers of epidermis (compared to upper surface layer), more accountable to present the underlying pathology given the cellular proliferation initiates from the basal layers and the upper layer uptake might be non-specific; and b) in non-violaceous central areas (compared to erythematous-violaceous peripheral areas), consistent with the pathophysiology of livedoid lesions given the vascular stenosis occurring in arterioles located in the center leads to livedo at the periphery.
To cite this abstract in AMA style:
Sevim E, Siddique S, Chalasani M, Chyou S, Shipman W, O`Shea O, Alpan O, Zuily S, Harp J, Lu T, Erkan D. Mammalian Target of Rapamycin (mTOR) Pathway Assessment in Antiphospholipid Antibody Positive Patients with Livedo Reticularis/Racemosa [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/mammalian-target-of-rapamycin-mtor-pathway-assessment-in-antiphospholipid-antibody-positive-patients-with-livedo-reticularis-racemosa-2/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/mammalian-target-of-rapamycin-mtor-pathway-assessment-in-antiphospholipid-antibody-positive-patients-with-livedo-reticularis-racemosa-2/