Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Products of oxidative stress, MAA adducts are highly immunogenic and have been associated with tolerance loss. To examine their potential role in disease-related inflammation, we investigated the presence of MAA adducts and circulating anti-MAA antibody in RA and their relationship with citrullinated proteins and anti-citrullinated protein antibody (ACPA).
Methods: Synovial tissues from RA and OA patients were examined for the presence of MAA-modified and citrullinated proteins. Anti-MAA antibody isotypes were measured in RA cases (n = 1720) and healthy controls (n = 80) by ELISA. Antigen-specific ACPA was measured in RA cases using a multiplex antigen array. Anti-MAA antibody isotype (IgG, IgM, and IgA) concentrations were compared in a subset of cases (n = 80) and controls (n = 80), matched based on age, gender, race, and smoking status. Associations of anti-MAA antibody isotypes with disease characteristics, including ACPA, were examined in all RA cases.
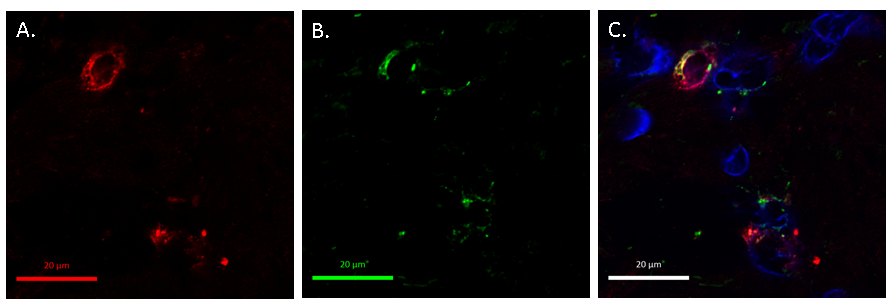
Results: MAA-adducted and citrullinated proteins were detected and shown to co-localize in RA synovial tissues (Fig. 1). In contrast, MAA adducts were present in negligible quantity while citrullinated proteins were absent in OA synovial tissue. All anti-MAA antibody isotypes were markedly increased in RA cases vs. controls (p < 0.001). Among RA cases, anti-MAA antibody isotypes were associated with anti-CCP antibody and RF positivity (p < 0.001) in addition to select measures of disease activity. Higher anti-MAA antibody concentrations were associated with a higher number of antigen-specific ACPA analytes positive in high titer (p < 0.001) and a higher ACPA score (p < 0.001), defined as the sum of normalized fluorescent values divided by the number of analytes examined (Fig. 2). Associations of anti-MAA antibody isotypes with ACPA score and the number of analytes positive were independent of other covariates.
Conclusion: This is the first study to show that MAA adduct formation is increased in RA and appears to result in robust antibody responses that are strongly associated with ACPA. These results support speculation that MAA adduct formation may be a co-factor that drives tolerance loss resulting in the autoimmune responses characteristic of RA.
Fig. 1: Immunohistochemical staining of RA synovial tissue demonstrated the presence of: a) citrullinated proteins, b) MAA, and c) co-localization of citrullinated proteins and MAA adducts
Fig. 2: Number of ACPA analytes positive (left) and total ACPA score (right) based on the quintile of circulating IgG anti-MAA antibody; similar results observed for IgA and IgM anti-MAA isotypes (data not shown).
Disclosure:
G. Thiele,
None;
M. J. Duryee,
None;
D. Anderson,
None;
L. W. Klassen,
None;
S. Mohring,
None;
K. Young,
None;
D. Benissan-Messan,
None;
H. Sayles,
None;
J. Sokolove,
None;
W. H. Robinson,
Atreca, Inc.,
5;
J. O’ Dell,
None;
A. Nicholas,
None;
T. R. Mikuls,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/malondialdehyde-acetaldehyde-adducts-maa-and-anti-malondialdehyde-acetaldehyde-antibody-in-rheumatoid-arthritis/