Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Palliative care is underutilized in patients with severe rheumatic disease. We sought to describe the perspectives of rheumatology and palliative care clinicians on the role palliative care in rheumatology.
Methods: Surveys for rheumatology and palliative care clinicians were created by adapting validated clinician attitude scales from the palliative care field to focus on rheumatology-specific care, with questions probing reasons for referral, barriers to referral, and comfort with palliative care skills. Surveys were distributed via email and in-person at local and national conferences to obtain responses from clinicians in different practice settings and geographic regions in the United States. Results were analyzed using descriptive statistics to identify patterns among demographic groups and clinician specialty.
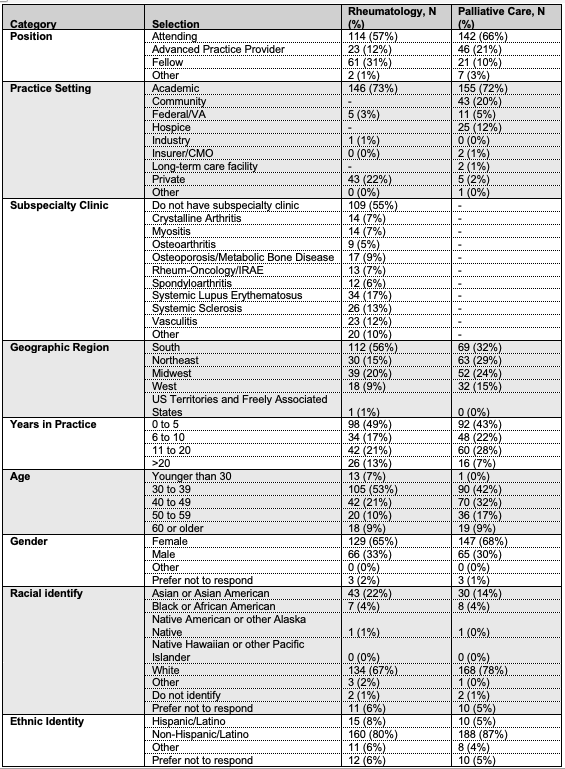
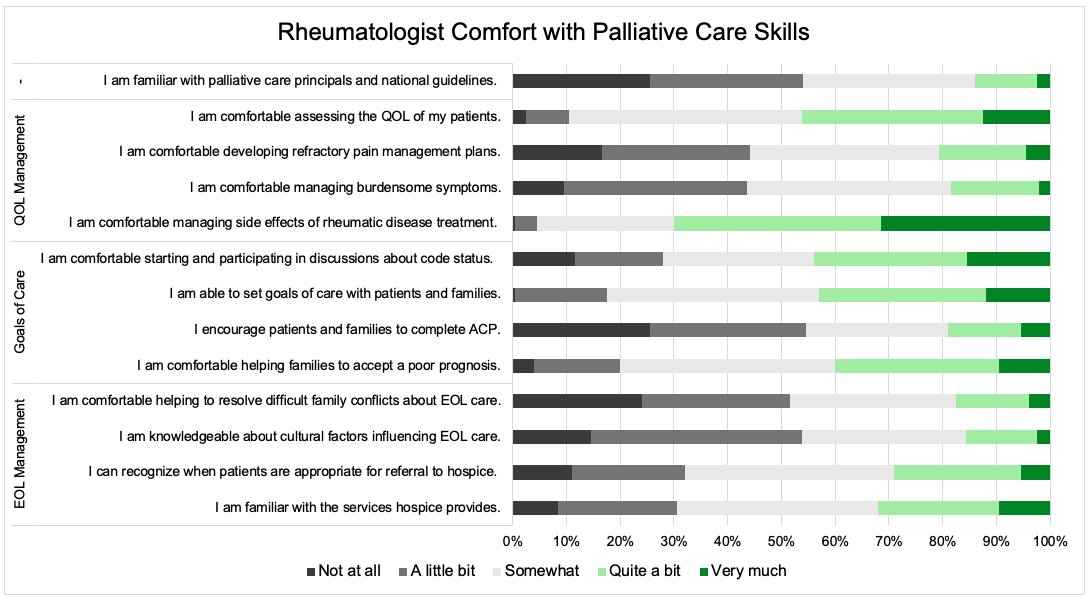
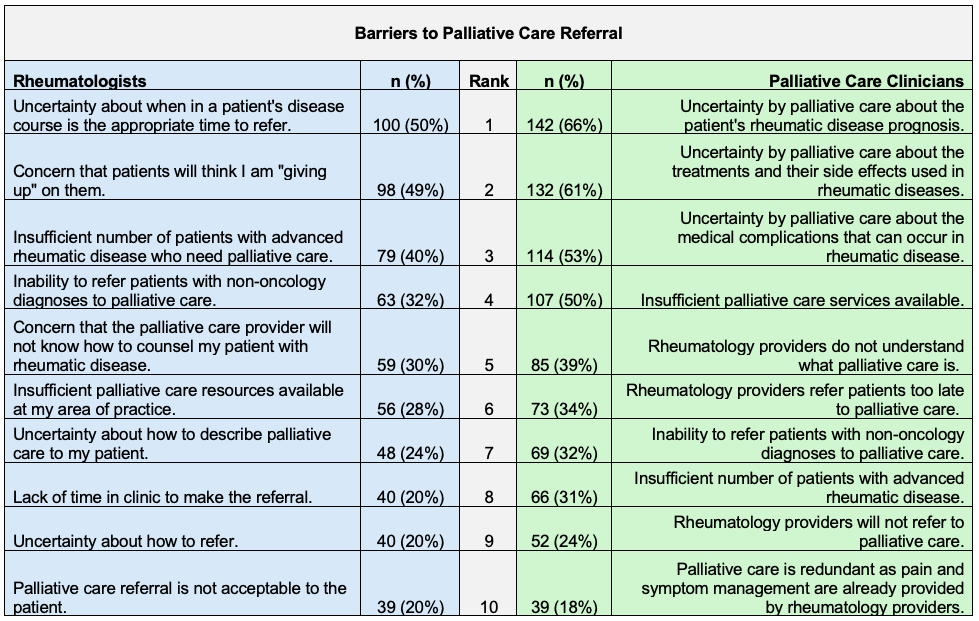
Results: 200 rheumatologists and 216 palliative care clinicians completed the survey (Table 1). Among rheumatologists, the majority reported never or rarely discussing advance care planning (ACP) (n=143, 72%), and many had not referred a patient to palliative care in the last year in the outpatient (n=135, 68%) or inpatient (n=95, 48%) setting. Despite this, the majority agreed or strongly agreed that more of their patients could benefit from palliative care (n=133, 67%), especially from a dedicated team specialized in palliative care pertaining to rheumatology (n=157, 79%). Only 4 (2.0%) rheumatology clinicians reported receiving education specifically about palliative care in rheumatology, and they reported low comfort with many pillars of palliative care (Figure 1). Among palliative care clinicians, the majority felt less comfortable providing care for rheumatology patients compared to other patients in their practice (n=163, 76%), and only 5 (2.3%) reported ever receiving education specifically about palliative care in rheumatology. Despite this, the majority felt they would be very or extremely helpful in common referral indications in patients with rheumatic disease, including patient and family support (n=175, 82%), symptom management (n=174, 81%), ACP (n=171, 79%), end-of-life care (n=167, 78%), and pain management (n=150, 70%). Regarding barriers to palliative care involvement for rheumatology patients, the top barriers for rheumatology clinicians were uncertainty about when to refer and concern that patients will think the clinician is “giving up” on them, whereas the top barriers for palliative care clinicians were related to rheumatology knowledge gaps (treatment side effects, prognosis, and complications of disease) (Table 2).
Conclusion: In summary, rheumatologists feel more of their patients would benefit from palliative care, though they rarely refer to palliative care and often do not feel comfortable providing primary palliative care themselves. Key barriers were identified. While palliative care clinicians feel they would be helpful caring for these patients, limited rheumatology knowledge is a barrier to care. These results identify major gaps in care of patients with severe rheumatic disease and provide a roadmap for further education, investigation, and collaboration between these specialties to better serve this patient population.
To cite this abstract in AMA style:
Herndon S, Kimball J, Jones C, Leverenz D. Making Rheum for Palliative Care in Rheumatology: Perspectives of Rheumatology and Palliative Care Clinicians [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/making-rheum-for-palliative-care-in-rheumatology-perspectives-of-rheumatology-and-palliative-care-clinicians/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/making-rheum-for-palliative-care-in-rheumatology-perspectives-of-rheumatology-and-palliative-care-clinicians/