Session Information
Session Type: ACR Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Ultrasonography is becoming an increasingly useful tool in evaluating patients in pediatric rheumatology. It is predominantly used for musculoskeletal assessments, however, major salivary gland ultrasound (SGUS) is being used in adults for assessment of primary and secondary Sjögren’s syndrome. Very few studies have been done examining salivary gland ultrasound in children and they have been confined to primary Sjögren’s syndrome. Examining children with rheumatic diseases who may be at risk for Sjögren’s syndrome such as childhood onset systemic lupus erythematosus (cSLE) may reveal early changes allowing for targeted intervention. Our primary objective is to determine acceptability and feasibility of SGUS in a pediatric rheumatology clinic. A secondary objective is to evaluate differences in ultrasound findings between cSLE Ro/La+ patients vs. cSLE Ro/La- patients.
Methods: Patients completed questionnaires rating symptoms of dryness, fatigue, pain, and reported any history of difficulty swallowing or episodic cheek swelling. Each patient underwent major SGUS of bilateral parotid glands (in two views) and bilateral submandibular glands (single view). Patients were asked to provide feedback on exam acceptability. Utilizing a previously published scoring system each major salivary gland image was scored by a blinded reviewer using a scale of 0-3 with a score of 0 representing a normal homogenous gland and a score of 3 representing diffuse gland heterogeneity. Scores of 2 or 3 were considered abnormal. The highest score was used as the overall ultrasound score for each patient. We used two sample independent t-tests or Fisher’s exact tests to compare disease factors and ultrasound scores between cSLE patients Ro/La+ vs. cSLE patients Ro/La-. A second analysis was performed to compare differences between cSLE patients with abnormal ultrasound score vs. cSLE patients with normal scores.
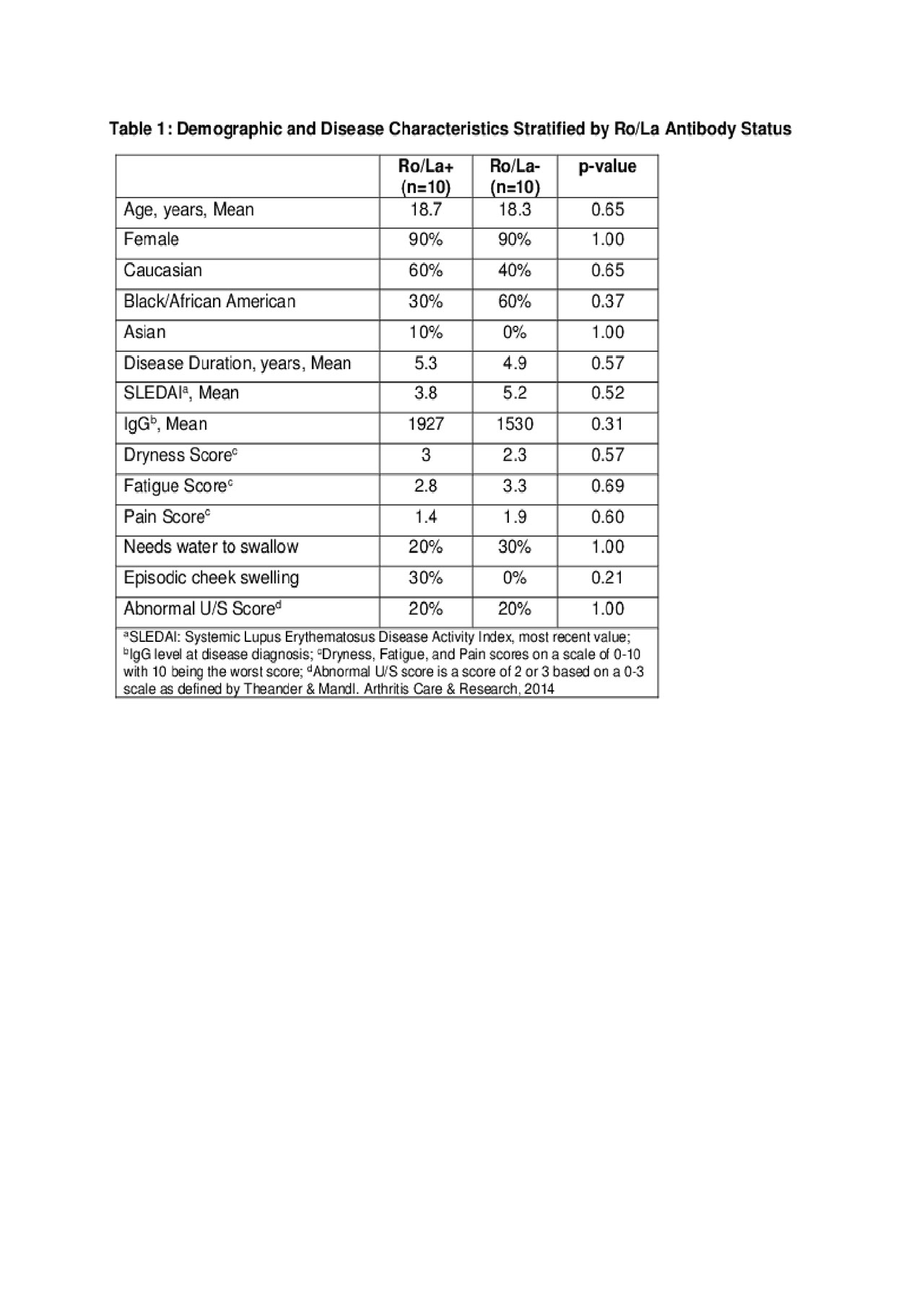
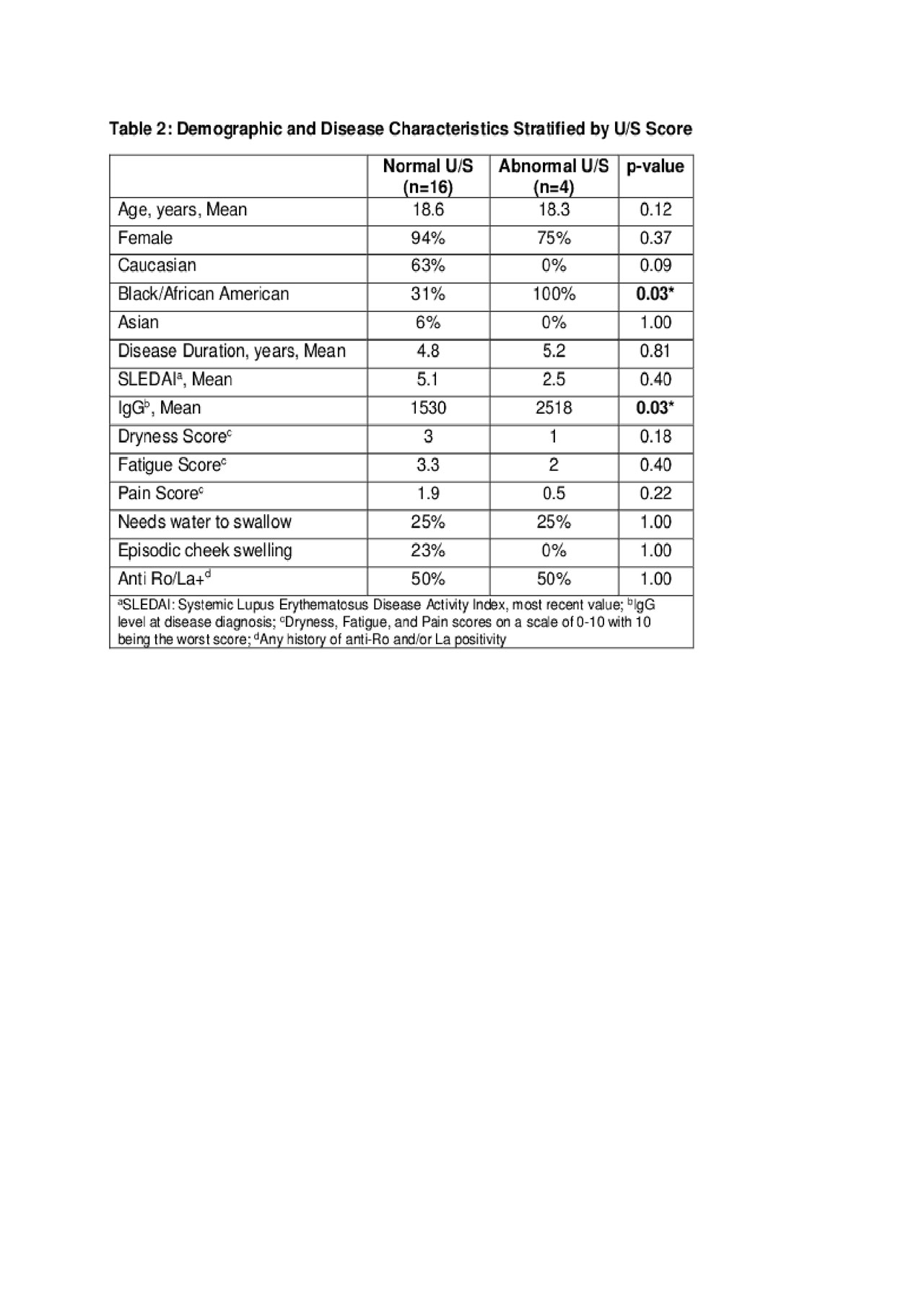
Results: Twenty cSLE patients were recruited, 90% were female, 50% were Caucasian. The average disease duration among all patients was 5 years. All twenty patients deemed the ultrasound examination acceptable. Average time to complete the ultrasound examination protocol was 4.5 minutes. No negative effects on clinic flow were reported. Age, gender, race, disease duration, SLEDAI, IgG level at diagnosis, dryness, fatigue, pain, and abnormal ultrasound scores did not differ between Anti-Ro/La+ cSLE patients compared to Anti-Ro/La- cSLE patients (Table 1). The data were also analyzed comparing patients with normal vs. abnormal SGUS scores. IgG level at diagnosis and Black race were significantly associated with abnormal SGUS scores (Table 2).
Conclusion: This is one of the first studies to assess major SGUS in a cohort of patients with cSLE. We demonstrate acceptability and feasibility of this ultrasound protocol performed by rheumatologists in a pediatric rheumatology clinic. Although the sample size was small we found SGUS abnormalities in 20% of patients. IgG level at diagnosis and Black race may predict risk for SGUS abnormalities. Larger cohort studies would be helpful to determine risk factors for SGUS abnormalities in children; ultimately leading to earlier diagnosis and treatment interventions.
To cite this abstract in AMA style:
McDonald J, Vega-Fernandez P, Ting T. Major Salivary Gland Ultrasound: Pilot Study of Findings and Feasibility in Childhood-Onset Systemic Lupus Erythematosus (cSLE) [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/major-salivary-gland-ultrasound-pilot-study-of-findings-and-feasibility-in-childhood-onset-systemic-lupus-erythematosus-csle/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/major-salivary-gland-ultrasound-pilot-study-of-findings-and-feasibility-in-childhood-onset-systemic-lupus-erythematosus-csle/