Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Progression of structural joint damage develops in 20-30 % of patients with rheumatoid arthritis (RA) in clinical remission1. Known predictors of structural damage progression in both active RA and in remission are magnetic resonance imaging (MRI)-detected synovitis and in particular osteitis/bone marrow edema (BME), but the predictive value of adding MRI tenosynovitis assessment as potential predictor in patients in clinical remission has not been investigated. The purpose was to investigate the predictive value of baseline MRI inflammatory and damage parameters on 2 year MRI and radiographic damage progression in an RA cohort in clinical remission, following MRI and conventional treat-to-target (T2T) strategies.
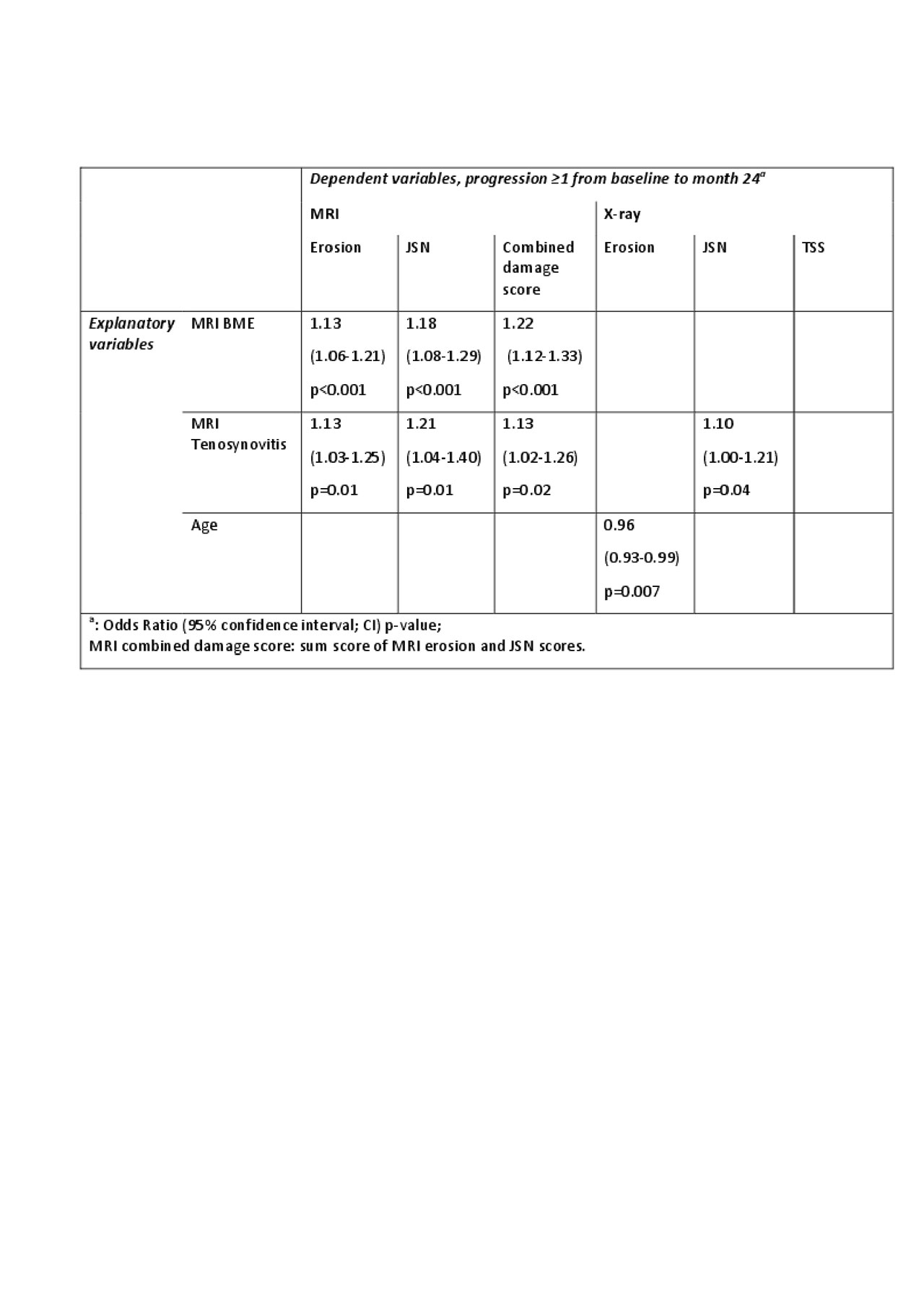
Methods: Two hundred RA patients in clinical remission, defined as DAS28-CRP< 3.2 and no swollen joints, on conventional DMARDs, were included in the IMAGINE-RA trial2. In this study patients were randomized to a conventional DAS28 + MRI-guided T2T strategy targeting absence of BME vs a conventional DAS28 guided T2T strategy. Patients had baseline and 2 years contrast-enhanced MRIs of the dominant wrist and 2nd-5th MCP joints and radiographs of hands and feet. Two experienced readers evaluated the MRIs and radiographs with known chronology according to the OMERACT RAMRIS scoring system and Sharp/van der Heijde method, respectively. The following potentially predictive baseline variables: MRI BME, synovitis, tenosynovitis, MRI and X-ray erosion and joint space narrowing (JSN) score, CRP, DAS28, smoking status, gender, age and patient group were tested in univariate logistic regression analyses with 2-year progression in MRI combined damage score, Total Sharp Score (TSS), and MRI and X-ray JSN and erosion scores as dependent variables. Variables with p< 0.1, age, gender and patient group were included in multivariable logistic regression analyses with backward selection.
Results: Based on univariate analyses MRI BME, synovitis, tenosynovitis, x-ray erosion and JSN, gender and age were included in subsequent multivariable analyses. Independent MRI predictors of structural progression were BME (MRI progression) and tenosynovitis (MRI and radiographic progression), see table.
Conclusion: This trial is the first to report that MRI tenosynovitis independently predicts both radiographic and MRI damage progression in RA patients in clinical remission. Further studies are needed to confirm MRI-determined tenosynovitis as predictor of progressive joint destruction in RA clinical remission.
References:
1) Lillegraven et al. Ann Rheum Dis 2012
2) Møller-Bisgaard et al. JAMA, 2019
ACR2019_abstract_IMAGINE_tenosynovitis_BME_predictor_of_damage_TABLE_20190603_FINAL_UPLOAD
To cite this abstract in AMA style:
Møller-Bisgaard S, Hørslev-Petersen K, Ejbjerg B, Lund Hetland M, Midtbøll Ørnbjerg L, Glinatsi D, Møller J, Boesen M, Stengaard-Pedersen K, Rintek Madsen O, Jensen B, Villadsen J, Hauge E, Bennett P, Hendricks O, Asmussen K, Kowalski M, Lindegaard H, Bliddal H, Krogh N, Ellingsen T, Nielsen A, Balding L, Jurik A, Thomsen H, Østergaard M. Magnetic Resonance Imaging in Patients in Clinical Remission: Tenosynovitis and Osteitis Are Independent Predictors of Radiographic and MRI Damage Progression [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/magnetic-resonance-imaging-in-patients-in-clinical-remission-tenosynovitis-and-osteitis-are-independent-predictors-of-radiographic-and-mri-damage-progression/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/magnetic-resonance-imaging-in-patients-in-clinical-remission-tenosynovitis-and-osteitis-are-independent-predictors-of-radiographic-and-mri-damage-progression/
